A pilot study to find the prevalence of diabetes mellitus among newly diagnosed pulmonary tuberculosis and individuals on anti-tuberculosis treatment
Abstract
Introduction: Diabetes Mellitus (DM) is a known risk factor of tuberculosis (TB). Moreover, the risk of getting TB is 3 times more among diabetics compared to the non-diabetics.
Materials and methods: Study was conducted in department of Microbiology, GSL Medical College, Rajahmundry. Individuals aged ≥ 18yeras were included in the study. The study participants were divided into two groups. Group A consist of newly diagnosed pulmonary tuberculosis (PT) individuals and individuals on anti tuberculosis treatment (ATT) were included in group B. Two spot sputum samples were collected from the participants, same day sputum collection approach; smear was stained by Ziehl Neelsen staining technique. Blood sample was collected and analyzed by HbA1C technique for sugar estimation.
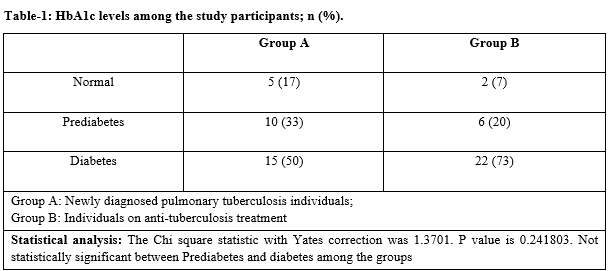
Results: In group A, 17%, 33% and 50% individuals were diagnosed to be normal, prediabetic and diabetic respectively. Whereas this was 7%, 20% and 73% respectively among group B. Age wise, individuals with diabetes were increased in both groups.
Conclusion: Diabetes is more among the individuals who are on ATT compared to newly diagnosed PT cases. Studies with large sample size are recommended.
Downloads
References
Chandra TJ. Same day sputum smear microscopy approach for the diagnosis of pulmonary tuberculosis in a microscopy center at Rajahmundry. Ind J Tuberc. 2012;59(3):141-144.
World Health Organization. Global tuberculosis report, 2014. WHO/HTM/TB/2014.08. Geneva, Switzerland: WHO, 2014. Available at https://apps.who.int/iris/handle/10665/137094.
Balakrishnan S, Vijayan S, Nair S, Subramoniapillai J, Mrithyunjayan S, Wilson N, et al. High diabetes prevalence among tuberculosis cases in Kerala, India. PLoS One. 2012;7:e46502. doi: https://doi.org/10.1371/journal.pone.0046502.
M Muñoz-Torrico M, Luna JC, Migliori GB, D’Ambrosio L, Carrillo-Alduenda JL, Villareal-Velarde H, et al. Comparison of bacteriological conversion and treatment outcomes among MDR-TB patients with and without diabetes in Mexico: Preliminary data. ReV Port Pneumol. 2017;23(1):27-30. doi: https://doi.org/10.1016/j.rppnen.2016.11.009.
Dooley KE, Chaisson RE. Tuberculosis and diabetes mellitus: convergence of two epidemics. Lancet Infect Dis. 2009;9(12):737-746. doi: https://doi.org/10.1016/S1473-3099(09)70282-8.
Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLos MED. 2008;5(7):e152. doi: https://doi.org/10.1371/journal.pmed.0050152.
Restrepo BI, Fisher-Hoch SP, Crespo JG, Whitney E, Perez A, Smith B, et al. Type 2 diabetes and tuberculosis in a dynamic bi-national border population. Epidemiol Infect. 2007;135(3):483-491. doi: https://doi.org/10.1017/S0950268806006935.
Wang CS, Yang CJ, Chen HC, et al. Impact of type 2 diabetes on manifestations and treatment outcome of pulmonary tuberculosis. Epidemiol Infect. 2009;137(2):203-210. doi: https://doi.org/10.1017/S0950268808000782.
Chang JT, Dou HY, Yen CL, Wu YH, Huang RM, Lin HJ. et al. Effect of type 2 diabetes mellitus on the clinical severity and treatment outcome in patients with pulmonary tuberculosis: a potential role in the emergence of multidrug resistance. J Formos Med Assoc. 2011;110(6):372-381. doi: https://doi.org/10.1016/S0929-6646(11)60055-7.
Zheng C, Hu M, Gao F. Diabetes and pulmonary tuberculosis: a global overview with special focus on the situation in Asian countries with high TB-DM burden. Global Health Action. 2017;10(1):1264702. doi: https://doi.org/10.1080/16549716.2016.1264702.
RNTCP (1998). Central TB Division. Manual for Laboratory Technicians. New Delhi, India: Directorate General of Health Services, Ministry of Health and Family Welfare, 1998. Available from: http://www.tbcindia.org/LABMANUAL.pdf [Last accessed date on 2017 Jan 22].
Chandra TJ, Selvaraj R., Sharma YV. Same-day sputum smear microscopy for the diagnosis of pulmonary tuberculosis: direct vs. concentrated smear. Int J Tuberc Lung Dis. 2016;20(2):247-251. doi: https://doi.org/10.5588/ijtld.15.0566.
Manjareeka M, Nanda S. Prevalence of HIV infection among tuberculosis patients in Eastern India. J Inf Public Health. 2013;5(6):358-362. doi: https://doi.org/10.1016/j.jiph.2013.04.004.
Olayinka AO, Anthonia O, Yetunde K. Prevalence of diabetes mellitus in persons with tuberculosis in a tertiary health centre in Lagos, Nigeria. Indian J Endocrinol Metab. 2013;17(3):486-489. doi: https://doi.org/10.4103/2230-8210.111646.
Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: A review of pathogene sis. Indian J Endocrinol Metab. 2012;16(1):S27-S36. doi: https://doi.org/10.4103/2230-8210.94253.
Viardot A, Grey ST, Mackay F, Chisholm D. Potential anti-inflammatory role of insulin via the preferential polarization of effector T cells toward a T helper 2 phenotype. Endocrinol. 2007;148(1):346-353. doi: https://doi.org/10.1210/en.2006-0686.
Stalenhoef JE, Alisjahbana B, Nelwan EJ, van der Ven-Jongekrijg J, Ottenhoff TH, van der Meer JW, et al. The role of interferon-gamma in the increased tuberculosis risk in type 2 diabetes mellitus. Eur J Clin Microbiol Infect Dis. 2008;27(2):97-103. doi: https://doi.org/10.1007/s10096-007-0395-0.
Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997;14(1):29-34.
Hongguang C, Min L, Shiwen J, Fanghui G, Shaoping H, Tiejie G, et al. Impact of diabetes on clinical presentation and treatment outcome of pulmonary tuberculosis in Beijing. Epidemiol Infect. 2015;143(1):150- 156. doi: https://doi.org/10.1017/S095026881400079X.
Viney K, Cavanaugh J, Kienene T, Harley D, Kelly PM, Sleigh A, et al. Tuberculosis and Diabetes Mellitus in the Republic of Kiribati: A Case-Control Study. Trop Med Int Health. 2015;20(5):650-657. doi: https://doi.org/10.1111/tmi.12462
Liu Q, Li W, Xue M, Chen Y, Du X, Wang C, et al. Diabetes mellitus and the risk of multidrug resistant tuberculosis: a meta-analysis. Scientific Rep. 2017;7(1):1090-1096. doi: https://doi.org/10.1038/s41598-017-01213-5.
International Union Against Tuberculosis and Lung Disease, World Health Organization. Collaborative framework for care and control of tuberculosis and diabetes. World Health Organization Document. WHO/HTM/TB/2011. 2011; 15: 1 – 40. Available at https://apps.who.int/iris/bitstream/handle/1066/4469/9789241502252_eng.pdf;jsessionid=882BA6197188A0D82A55BFE57A18004D?sequence=1.
Manjareeka M, Palo SK, Swain S, Pati S, Pati S. Diabetes Mellitus among Newly Diagnosed Tuberculosis Patients in Tribal Odisha: An Exploratory Study. J Clin and Diag Res. 2016;10(10):LC06-LC08. doi: https://doi.org/10.7860/JCDR/2016/20999.8704
Hoa NB, Phuc PD, Hien NT, Hoa VQ, Thuong PH, Anh PT et al. Prevalence and associated factors of diabetes mellitus among tuberculosis patients in Hanoi, Vietnam. BMC Infect Dis. 2018;18(1):603-612. doi: https://doi.org/10.1186/s12879-018-3519-5
Workneh MH, Bjune GA, Yimer SA. Prevalence and associated factors of diabetes mellitus among tuberculosis patients in South-Eastern Amhara region, Ethiopia: a cross sectional study. PLoS One. 2016;11(1): e0147621. doi: https://doi.org/10.1371/journal.pone.0147621.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


