Cytological spectrum of lymph node lesions-our institute experience
Abstract
Introduction: Lymphadenopathy is of great clinical significance as underlying diseases may range from a treatable infectious etiology to malignant neoplasms. Fine needle aspiration cytology (FNAC) plays a vital role in solving these issues, being recognised as rapid diagnostic technique because of simplicity accuracy and minimal invasion.
Aim: To know the cytological spectrum of lymphadenopathy and to understand the burden of disease in this region. Design: This is a retrospective cytological study on 1478 patients including all age groups and both genders presenting with palpable lymphadenopathy over a period of seven years.
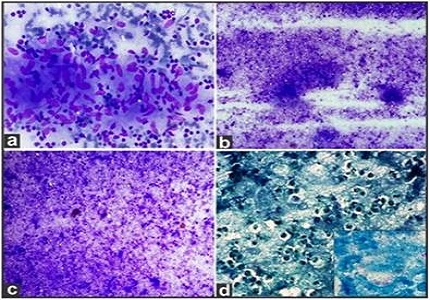
Materials and Methods: FNAC was conducted with 22-24 gauge needle attached to 20 cc syringes. Smears were stained with Giemsa and Papanicolaou stains routinely; and special stains like Zeihl-Neelsen and periodic acid-Schiff were done whenever required. The data were tabulated as per the involvement of various lymph node groups and type of neoplastic and non-neoplastic lesions involved. Data was analysed using SPSS 22 version.
Results: Out of 1478 aspirations of lymph nodes, the most frequent cause of lymphadenopathy was found to be tuberculous lymphadenitis 592 (40.06%) cases. The next frequent diagnosis was reactive lymphadenopathy with 550 (37.2%) cases, followed by metastatic lymphadenopathy in 243 (16.4%) cases. The diagnosis of primary neoplastic lesions was seen in 29 (2.0%) cases.
Conclusion: In our study, the predominant cause of lymphadenopathy was tuberculous lymphadenitis, followed by reactive lymphadenopathy and malignant neoplasms especially metastatic carcinoma. FNAC was helpful in diagnosing approximately 98% of cases.
Downloads
References
2. Cohen MB, Miller TR, Bottles K. Classics in cytology: note on fine needle aspiration of the lymphatic glands in sleeping sickness. Acta Cytol. 1986 Jul-Aug;30(4):451-2. [PubMed]
3. Wilkinson AR, Mahore SD, Maimoon SA. FNAC in the diagnosis of lymph node malignancies: A simple and sensitive tool. Indian J Med PaediatrOncol. 2012 Jan;33(1):21-4. doi: 10.4103/0971-5851.96964. [PubMed]
4. Sharma P, Rana S, Gill MK, Singh P, Satarkar RN, Kalhan. Spectrum of lymph node lesions on cytology in rural Haryana: a retrospective analysis. Int J Res Med Sci. 2015; 3(5): 1125-30. doi: 10.5455/2320-6012.ijrms20150518.
5. Singh JP, Chaturvedi NK, Das A. Role of Fine needle aspiration cytology in the diagnosis of tuberculous lymphadenitis. Indian J PatholMicrobiol. 1989; 32:100-4.
6. Pavithra P, Geetha JP. Role of fine needle aspiration cytology in the evaluation of the spectrum of lymph node lesions. Int J Pharm Bio Sci. 2014;5(4):377-84.
7. Dukare SR, Jadhav DS, Gaikwad AL, Ranka SN, Kale PB, D’Costa G. Fine needle aspiration cytology of cervical lymphadenopathy - a study of 510 cases. Asian J Sci Technol. 2014; 5(9):537-40.
8. Pandav AB, Patil PP, Lanjewar DN. Cervical lymphadenopathy diagnosis by FNAC: a study of 219 cases. Asian J Med Res. 2012; 1(3):79-83.
9. Rajshekaran S. Tuberculous cervical lymphadenitis in HIV positive and negative patients. Indian J Tuberc. 2001; 48:201-4.
10. Chandanwale S, Buch A, Verma A, Shruthi V, Kulkarni S, Satav V. Evaluation of granulomatous lymphadenitis on fine needle aspiration cytology - diagnostic dilemma. Int J Pharm Bio Sci. 2014; 5(4):377-84.
11. Patel MM, Italiya SL, Patel RD, Dudhat RB, Kaptan KR, Baldwa VM. Role of fine needle aspiration cytology to analyse various causes of lymphadenopathy. National J Community Med. 2013; 4(3): 489-492.
12. Giri S, Singh K. Role of fine needle aspiration cytology in evaluation of patients with superficial lymphadenopathy. Int J Biol Med Res. 2012; 3(4): 2475-9.
13. Tilak V, Dhaded AV, Jain R. Fine needle aspiration cytology of head and neck masses. Indian J PatholMicrobiol. 2002 Jan;45(1):23-9. [PubMed]
14. Kocchar A, Duggal G, Singh, Kocchar S. Spectrum of cytological findings in patients with lymphadenopathy in rural population of Southern Haryana, India- Experience in a tertiary care hospital. The Internet J Pathol. 2012; 13(2): 1-6.
15. Mohanty R, Wilkinson A. Utility of fine needle aspiration of lymph nodes. IOSR J Dent Med Sci. 2013; 8(5):13-8.
16. Fatima S, Arshad S, Ahmed Z, Hasan SH. Spectrum of cytological findings in patients with neck lymphadenopathy- Experience in a tertiary care hospital in Pakistan. Asian Pacific J Cancer Prevention. 2011; 12: 1873-5.
17. Chand P, Dogra R, Chauhan N, Gupta R, Khare P. Cytological pattern of tubercular lymphadenopathy on FNAC: analysis of 550 consecutive cases. J ClinDiagn Res. 2014; 8(9):FC16-9. doi:10.7860/JCDR/2014/9956.4910.
18. Kline TS, Khannan V, Line IK. Lymphadenopathy and aspiration biopsy cytology review of 376 superficial lymphnodes. Cancer. 1984; 54:1076-81.
19. Hemlatha A, Udaya Kumar M, Harendra Kumar ML. Fine needle aspiration cytology of lymph nodes: A mirror in the diagnosis of spectrum of lymph node lesons. J Clin Biomed Sci 2011; 1:164-72.
20. Vimal S, Dharwadkar A, Chandanwale SS, Vishwanathan V, Kumar H. Cytomorphological study of lymph node lesions: A study of 187 cases. Med J DY Patil Univ. 2016; 9: 43-50. doi:10.4103/0975-2870.172428.
21. Bezabih M, Marian DW, Selassie SG. Fine needle aspiration cytology of cervical lymphadenopathy with special reference to tuberculosis. J Indian Med Assoc. 1994; 92:44-6. [PubMed]
22. Paliwal N, Thakur S, Mullick S, Gupta K. FNAC in tuberculous lymphadenitis: experience from a tertiary level referral centre. Indian J Tuberc. 2011; 58:102-7. [PubMed]
23. Aggarwal P, Wali JP, Singh S, HandaR, Wig N, Biswas A. A clinico bacterial study of Peripheral tuberculous lymphadenitis. J Assoc Physicians India. 2001; 49:808-12.
24. Das DK. Fine needle aspiration cytology in the diagnosis of tuberculous lesions. Lab Med. 2003; 31(11):625-32.
25. Bhardwaj K, Goyal T, Bhardwaj BL. Fine needle aspiration cytology in lymph node disorders with special reference to tuberculosis. J Cytol. 2000; 17(3):155-9.
26. Lau SK, Wei WI, Hsu C, Engzell UC. Efficacy of fine needle aspiration cytology in the diagnosis of tuberculous cervical lymphadenopathy. J Laryngol Otol. 1990 Jan;104(1):24-7.
27. Khajuria R, Goswami KC, Singh k, Dubey VK. Pattern of lymphadenopathy on fine needle aspiration cytology in Jammu. JK Science. 2006; 8(3): 157-9.
28. Patra AK, Nanda BK, Mohapatra BK, Panda AK. Diagnosis of lymphadenopathy by fine needle aspiration cytology. Indian J PatholMicrobiol. 1983 Oct;26(4):273-8.
29. Hafez NH, Tahoun NS. Reliability of fine needle aspirationcytology (FNAC) as a diagnostictool in cases of cervicallymphadenopathy. JEgyptNatlCancInst. 2011 Sep;23(3):105-14. doi: 10.1016/j.jnci.2011.09.009. Epub 2011 Oct 24. [PubMed]


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


