Incidence of H1N1 in pediatric population in a tertiary care hospital in Bangalore
Abstract
Objectives: Influenza viruses continue to be a major health threat in both endemic and pandemic forms. The rapid, continuous, and unpredictable nature of influenza viral evolution makes vaccine strategies and pandemic planning difficult .In elderly, infants and in people with chronic diseases, influenza is associated with high mortality. As there are very limited studies relating to Influenza A H1N1 and its epidemiology in the pediatric population, this study was done to study the clinical and epidemiological profile of patients found positive for Influenza A H1N1 in pediatric population in a tertiary care hospital in Bangalore.
Materials and methods: This is a retrospective study done over a period of 6 months from January 2017 to June 2017. The study population included all the suspected patients tested for Influenza A H1N1 by real-time RT-PCR.
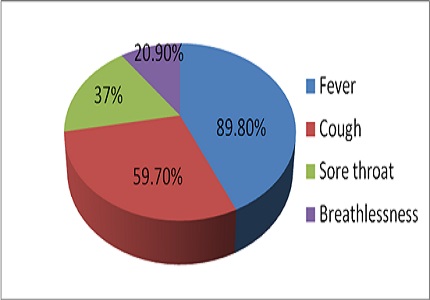
Results: Total of 89 patients were tested for Influenza A H1N1 out of which 31(34.8%) were positive. The most common symptoms were fever (87.6%), cough (49.77%), sore throat (27%) and breathlessness (23.9%). Maximum cases were detected in the 0-5 years age group in that 19(61.2%) were positive, followed by 15-18 yrs in which 23(25.8%) were tested in which 9(29.03%) were positive. Influenza A H1N1 resulted in death of 3(3.3%) of the total admitted suspected H1N1 cases in our hospital.
Conclusion: On the basis of these findings, it can be concluded that prevalence of Influenza A H1N1 is high in children with the age group of 0-5yrs. The age shift of severe influenza A (H1N1) towards younger children may be explained by increasing immunity in the older pediatric population.
Downloads
References
2. Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL, Daszak P. Global trends in emerging infectious diseases. Nature. 2008 Feb 21;451(7181):990-3. doi: 10.1038/nature06536. [PubMed]
3. Bhatt KN, Jethw SC, Bhadiyadar D, Patel D, Joshi K. Study of clinical profile in patients with H1N1 influenza in Surat district, June 2009 – March 2010. J Assoc Physicians India 2012;60:15-9.
4. Sharma R, Agarwal S, Mehta S, Nawal CL, Bhandari S, Rathore M, et al. Profiling the mortality due to influenza A (H1N1) pdm09 at a tertiary care hospital in Jaipur during the current season--January & February 2015. J Assoc Physicians India 2015;63:36-9.
5. Nadkar MY, Subramanian S, Ingole N. H1N1 influenza: An update. JAPI 2009;57:454-8.
6. Centers for Disease Control and Prevention (CDC). Update: influenza activity--United States and worldwide, 1999-2000 season, and composition of the 2000-01 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2000 May 5;49(17):375-81.
7. Heikkinen T. Influenza in children. Acta Paediatr. 2006 Jul;95(7):778-84. [PubMed]
8. Poehling KA, Edwards KM, Weinberg GA, Szilagyi P, Staat MA, Iwane MK, Bridges CB, Grijalva CG, Zhu Y, Bernstein DI, Herrera G, Erdman D, Hall CB, Seither R, Griffin MR; New Vaccine Surveillance Network. The underrecognized burden of influenza in young children. N Engl J Med. 2006 Jul 6;355(1):31-40.
9. Quach C, Piché-Walker L, Platt R, Moore D. Risk factors associated with severe influenza infections in childhood: implication for vaccine strategy. Pediatrics. 2003;112:197–201. doi: 10.1542/peds.112.3.e197.
10. Wong KK, Jain S, Blanton L, Dhara R, Brammer L, Fry AM, Finelli L. Influenza-associated pediatric deaths in the United States, 2004-2012. Pediatrics. 2013 Nov;132(5):796-804. doi: 10.1542/peds.2013-1493. Epub 2013 Oct 28. [PubMed]
11. Gill PJ, Ashdown HF, Wang K, Heneghan C, Roberts NW, Harnden A, et al. Identification of children at risk of influenza-related complications in primary and ambulatory care: a systematic review and meta-analysis. Lancet Respir Med. 2015;3:139–49. doi: 10.1016/S2213-2600(14)70252-8. [PubMed]
12. Ruf BR, Knuf M. The burden of seasonal and pandemic influenza in infants and children. Eur J Pediatr. 2014 Mar;173(3):265-76. doi: 10.1007/s00431-013-2023-6. Epub 2013 May 10.
13. Neuzil KM, Wright PF, Mitchel EF, Jr, Griffin MR. The burden of influenza illness in children with asthma and other chronic medical conditions. J Pediatr. 2000;137:856–64. doi: 10.1067/mpd.2000.110445.
14. Louie JK, Schechter R, Honarmand S, Guevara H, Shoemaker TR, Madrigal NY, et al. Severe paediatric influenza in California, 2003–2005: implications for immunization recommendations. Pediatrics. 2006;117:e610–8. doi: 10.1542/peds.2005-1373.
15. Çiftçi E, Tuygun N, Özdemir H, Tezer H, Şensoy G, Devrim İ et al .Clinical and epidemiological features of Turkish children with 2009 pandemic influenza A (H1N1) infection: experience from multiple tertiary paediatric centres in Turkey. 2009-2011Scand J Infect Dis. 2011 Dec;43(11-12):923-9. doi: 10.3109/00365548.2011-598872.
16. Fitzgerald DA. Human swine influenza A [H1N1]: practical advice for clinicians early in the pandemic. Paediatr Respir Rev. 2009 Sep;10(3):154-8. doi: 10.1016/j.prrv.2009.06.005. Epub 2009 Jul 16. [PubMed]
17. Novel Swine-Origin Influenza A (H1N1) Virus Investigation Team, Dawood FS, Jain S, Finelli L, Shaw MW, Lindstrom S, Garten RJ, Gubareva LV, Xu X, Bridges CB, Uyeki TM. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009 Jun 18;360(25):2605-15. doi: 10.1056/NEJMoa0903810. Epub 2009 May 7. [PubMed]
18. Witkop CT, Duffy MR, Macias EA, Gibbons TF, Escobar JD, Burwell KN, Knight KK. Novel Influenza A (H1N1) outbreak at the U.S. Air Force Academy: epidemiology and viral shedding duration. Am J Prev Med. 2010 Feb;38(2):121-6. doi: 10.1016/j.amepre.2009.10.005. Epub 2009 Oct 21.
19. Hackett S, Hill L, Patel J, Ratnaraja N, Ifeyinwa A, Farooqi M, Nusgen U, Debenham P, Gandhi D, Makwana N, Smit E, Welch S. Clinical characteristics of paediatric H1N1 admissions in Birmingham, UK. Lancet. 2009 Aug 22;374(9690):605. doi: 10.1016/S0140-6736(09)61511-7.
20. Hayden FG, Gubareva LV, Monto AS, Klein TC, Elliot MJ, Hammond JM, et al. Inhaled zanamivir for the prevention of influenza in families. Zanamivir Family Study Group. N Engl J Med. 2000 Nov 2. 343(18):1282-9.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


