Causative Organisms and associated antimicrobial resistance in Central Line-Associated Blood Stream Infections from patients admitted in ICU of tertiary health care hospital of Jammu region.
Abstract
Introduction: CLABSI (Central Line Associated Bloodstream Infection) is the presence of bacteremia originating from a central line catheter. CLABSI is a common cause of health care associated infection, and is a major cause of morbidity and mortality. We did this study to study the incidence, bacteriological profile and antimicrobial susceptibility pattern of the isolates in CLABSI in the Intensive Care Unit (ICU) patients.
Material and methods: This prospective study was conducted for one year in Department of Microbiology on patients admitted in ICU for more than 48 hours with Central line catheter. The CLABSI rate was calculated. The formula for CLABSI Rate used was CLABSI incidence rate which was calculated as no. of CLABSI / no. of central line days × 1000.
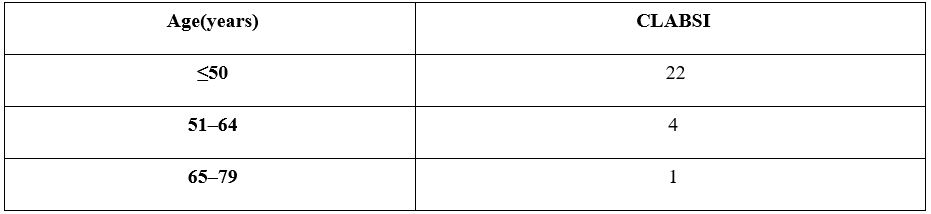
Results: Out of 448 patients 306 have central line. Out of 306 patients 140 develop symptoms related to device associated infections. Among 140 patients 27 develop central line associated blood stream infection. The CLABSI rate found was 17.76 per 1000 catheter days. Staphylococcus aureus was the most common pathogen isolated among gram positive cocci. Among gram negative bacilli was Acinetobacter sp. Multi drug resistance was seen in the first line of antibiotics used.
Conclusion: CLABSI had a significant impact on the overall healthcare costs. Knowledge about risk factors and infection control measures for CLABSI prevention is crucial for best clinical practice.
Downloads
References
2. Merzel LA. Prevention of intravascular catheter-related infections. Ann Intern Med 2000; 132:391–402.
3. Saxena AK and Panhotra BR. Haemodialysis catheter-related bloodstream infections: current treatment options and strategies for prevention. Swiss Med Wkly2005; 135(9 -10):127–38.
4. Dudeck MA et al. NHSN 2013 HAI data: National Healthcare Safety Network report, data summary for 2013, device associated module. Am j infect control 2015; 43:206-
21.
5. SinghS, ChakravarthyM, SenguptaS, MunshiN, JoseT, ChayaV. Analysis of a multicentric pooled healthcare associated infection data from India: New insights. J Natl
Accredit Board Hosp Health Provid2014; 1:39
6. Sastry A, Deepshree R. Major Healthcare-associated Infection Types: Text Book of Essentials of Hospital Infection Control, 1stedn. New Delhi: Jaypee Brothers Medical Publishers; 2019.p.15-69.
7. Pitout JDD, Laupland KB. Extended-spectrum β-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis 2008; 8:159–66.
8. Fridkin SK, Hageman JC, Morrison M, et al. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med 2005; 352:1463–44.
9. Klevens RM, Morrison MA, Nadle J, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 2007; 298:1763–71.
10. Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. Available at: http://www.cdc.gov/drugresistance/threatreport2013/. Accessed 10 March 2016.
11. Centers for Disease Control and Prevention. Vital signs: carbapenem-resistant Enterobacteriaceae. MMWR Morb Mortal Wkly Rep 2013; 62:165–70.
12. Kuo SH, Lin WR, Lin JY, et al. The epidemiology, antibiograms and predictors of mortality among critically-ill patients with central line-associated bloodstream infections. J Microbiol Immunol Infect 2018;51:401–10.
13. Kaur M, Gupta V, Gombar S, et al. Incidence, risk factors, microbiology of venous catheter associated bloodstream infections - a prospective study from a tertiary care hospital. Indian J Med Microbiol 2015;33:248–54.
14. Bell T, O'Grady NP. Prevention of Central Line-Associated Bloodstream
Infections. Infect Dis Clin North Am. 2017; 31(3):551-59.
15. Soundaram GVG, Sundaramurthy R, Jeyashree K, Ganesan V, Arunagiri R, Charles J. Impact of Care Bundle Implementation on Incidence ofCatheter-associated
Urinary Tract Infection: A ComparativeStudy in the Intensive Care Units of a Tertiary Care TeachingHospital in South India. Indian J Crit Care Med 2020; 24(7):544–550.
16. Yoshida T, Silva AEBC, Simões LLP, Guimarães RA. Incidence of Central Venous Catheter-Related Bloodstream Infections: Evaluation of Bundle Prevention in Two Intensive Care Units in Central Brazil. Scientific World Journal. 2019 Oct 7; 2019:1025-032.
doi: 10.1155/2019/1025032.PMID: 31687000; PMCID: PMC6800912.
17. Salama MF , Jamal W, Mousa HAI, Rotimib V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: Effect on centralline-associated bloodstream infections. Journal of Infection and Public Health 2016; 9:34-41.
18. Sun Y, Bao Z, Guo Y, Yuan X. Positive effect of care bundles on patients with central venous catheter insertions at a tertiary hospital inBeijing, China. Journal of International Medical Research 2020; 48(7):1–10.
19. Deron C et al. Methicillin-Resistant Staphylococcus aureus Central Line–Associated Bloodstream Infections in US Intensive Care Units, 1997-2007. Journal of the American Medical Association (JAMA), February 18, 2009—Vol 301, No. 7
20. Litwin A et al.Pseudomonas aeruginosa device associated – healthcare associated infections and its multidrug resistance at intensive care unit of University Hospital: polish, 8.5-year, prospective, single-centre study. BMC Infectious Diseases (2021);21:180
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


