Fungal profile of sputum samples and their Anti-Fungal Susceptibility profile in a Tertiary care Hospital in Sikkim.
Abstract
Abstract:
Introduction: The significance of fungal growth in sputum culture remains uncertain and is typically not addressed when detected. This study aims to outline the clinical observations of individuals exhibiting fungal growth in their sputum, as well as assess their susceptibility to antifungal agents. The primary objective is to acquire an understanding of the local epidemiology related to resistance against antifungal agents.
Material and method: This is a hospital-based, cross-sectional study conducted for a period of one year January-December 2022 in a Tertiary care hospital in Sikkim. Sputum samples from in-Patients (ICU/Ward) were processed for fungal culture and the identification was done by Chrome Candida differential agar and the automated Microbiology System for yeast and yeast-like organisms, the moulds were identified morphologically. Anti-fungal susceptibility testing (AFST) was done using antifungal disks Amphotericin B 20 mcg, Itraconazole 10 mcg, Fluconazole 25mcg and Voriconazole 1 mcg and following Standard operating procedure (SOP) manual of ICMR 2nd edition 2019.
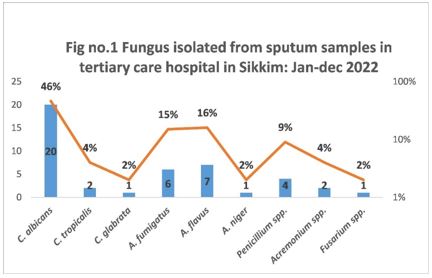
Results: Out of 190 samples, 23(12%) and 21 (11%) Candida spp. and moulds were isolated. Among Candida spp., Candida albicans was isolated in 20, Candida tropicalis in 2 , and Candida. glabrata in 1. AFST showed 91% of Candida spp. were sensitive to Amphotericin B followed by Fluconazole (39%) and Voriconazole (35%). Among 21 moulds identified A. fumigatus (6), A. flavus (7), A. niger (1), Penicillium spp. (4), Acremonium spp. (2) and Fusarium spp. (1) were isolated. AFST showed that Voriconazole was the most sensitive (85%) followed by Amphotericin B (57%) and the most resistant antifungal was Fluconazole (71%) followed by Itraconazole (47%) in moulds. frr
Conclusion: The study brought attention to prevalent fungal commensals within the respiratory tract and provided insights into the susceptibility patterns of fungal pathogens in the region.
Downloads
References
1. de S Araújo GR, Souza W, Frases S. The hidden pathogenic potential of environmental fungi. Future Microbiol. 2017 12:1533-40. doi: 10.2217/fmb-2017-0124. Epub 2017 - 23. PMID: 29168657.
2. Limper AH, Knox KS, Sarosi GA, Ampel NM, Bennett JE, Catanzaro A , et al. American Thoracic Society Fungal Working Group. An official American Thoracic Society statement: Treatment of fungal infections in adult pulmonary and critical care patients. Am J Respir Crit Care Med. 2011 1;183(1):96-128. doi: 10.1164/rccm.2008-740ST. PMID: 21193785.
3. Valerio M, Rodriguez-Gonzalez CG, Muñoz P, Caliz B, Sanjurjo M, Bouza E; COMIC Study Group (Collaborative Group on Mycoses) Evaluation of antifungal use in a tertiary care institution: antifungal stewardship urgently needed. J Antimicrob Chemother 2014; 69:1993–9.
4. Rafat Z, Hashemi SJ, Ashrafi K, Nikokar I, Jafari A, Rahimi Foroushani A , et al. Fungal Isolates of the Respiratory Tract in Symptomatic Patients Hospitalized in Pulmonary Units: A Mycological and Molecular Epidemiologic Study. J Multidiscip Healthc. 2020 Jul 22; 13:661-669. doi: 10.2147/JMDH.S252371. PMID: 32801730; PMCID: PMC7383022.
5. Biswas D, Agarwal S, Sindhwani G, Rawat J. Fungal colonization in patients with chronic respiratory diseases from Himalayan region of India. Ann Clin Microbiol Antimicrob. 2010 20; 9:28. doi: 10.1186/1476-0711-9-28. PMID: 20854652; PMCID: PMC2949792.
6. Phukan AC, Sarmabordoloi JN, Mahanta J. Bronchopulmonary candidiasis in a tertiary referral hospital of Assam, India. Indian J Med Sci. 2000 ;54(11):491-4. PMID: 11354809.
7. Ghaddar N, Anastasiadis E, Halimeh R, Ghaddar A, Dhar R, AlFouzan W, et al. Prevalence and antifungal susceptibility of Candida albicans causing vaginal discharge among pregnant women in Lebanon. BMC Infect Dis. 2020 13;20(1):32. doi: 10.1186/s12879-019-4736-2. PMID: 31931738; PMCID: PMC6958632
8. Zeng ZR, Tian G, Ding YH, Yang K, Liu JB, Deng J. Surveillance study of the prevalence, species distribution, antifungal susceptibility, risk factors and mortality of invasive candidiasis in a tertiary teaching hospital in Southwest China. BMC Infect Dis. 2019 7;19(1):939. doi: 10.1186/s12879-019-4588-9. PMID: 31699043; PMCID: PMC6836498.
9. Vazquez JA, Arganoza MT, Vaishampayan JK, Akins RA. In vitro interaction between amphotericin B and azoles in Candida albicans. Antimicrob Agents Chemother. 1996;40(11):2511-6. doi: 10.1128/AAC.40.11.2511. PMID: 8913455; PMCID: PMC163566.
10. Pérez-Cantero A, López-Fernández L, Guarro J, Capilla J. Azole resistance mechanisms in Aspergillus: update and recent advances. Int J Antimicrob Agents. 2020;55(1):105807. doi: 10.1016/j.ijantimicag.2019.09.011. Epub 2019 Sep 19. PMID: 31542320.
11. Paul RA, Rudramurthy SM, Dhaliwal M, Singh P, Ghosh AK, Kaur H, et al . Magnitude of Voriconazole Resistance in Clinical and Environmental Isolates of Aspergillus flavus and Investigation into the Role of Multidrug Efflux Pumps. Antimicrob Agents Chemother. 2018 24;62(11):e01022-18. doi: 10.1128/AAC.01022-18. PMID: 30126956; PMCID: PMC6201112.
12. Pfaller M, Boyken L, Hollis R, Kroeger J, Messer S, Tendolkar S, et al. Use of epidemiological cutoff values to examine 9-year trends in susceptibility of Aspergillus species to the triazoles. J Clin Microbiol. 2011 Feb;49(2):586-90. doi: 10.1128/JCM.02136-10. Epub 2010 1. PMID: 21123534; PMCID: PMC3043512.
13. Paul RA, Rudramurthy SM, Dhaliwal M, Singh P, Ghosh AK, Kaur H, et al . Magnitude of Voriconazole Resistance in Clinical and Environmental Isolates of Aspergillus flavus and Investigation into the Role of Multidrug Efflux Pumps. Antimicrob Agents Chemother. 2018 24;62(11):e01022-18. doi: 10.1128/AAC.01022-18. PMID: 30126956; PMCID: PMC6201112.
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


