Estimation of NLR in COVID-19 Patients in a Tertiary Care Center& determining its significance as a prognostic marker
Abstract
Introduction: The rapid spread and serious harm of COVID-19 makes it urgent to continuouslyimprove and enrich its clinical diagnosis and treatment research. Using a simple test like NLR forassessing the risk of mortality and early identification of severe cases will help in preventing life-threatening complications in COVID-19 patients. Objectives: To study trends of NLR counts inCOVID 19 patients and the correlation between NLR and COVID-19 severity.
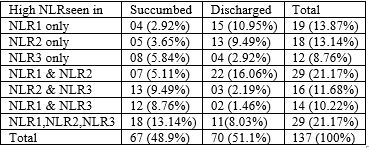
Methods: A total of137 random subjects whose blood samples were collected on the day of admission, on the 3rd dayand on the 6th day of admission were included in the study. NLR was calculated as simplyneutrophils /lymphocytes and trends were studied.
Results: An average of all three NLR counts forthe patients revealed an overall decreasing trend in cases of survivors, whereas an overall upwardtrend was noted in the non-survivors. All of the patients admitted to the COVID ICU, that is thosewho had severe disease, showed a high NLR value of >3, in at least one of the three tests.
Conclusion: The NLR was the most promising predictive factor for critical illness incidence ofCOVID-19 pneumonia. Early application of NLR will be beneficial for patient management and reliefof medical resource shortage.
Downloads
References
2. Lu H, Stratton CW, Tang Y‐W. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol. 2020;92:401–402. 10.1002/jmv.25678
3. Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. IntImmunopharmacol. 2020;84:106504. doi:10.1016/j.intimp.2020.106504
4. Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-733. doi:10.1056/NEJMoa2001017
5. Xiang N, Havers F, Chen T, et al. Use of national pneumonia surveillance to describe influenza A(H7N9) virus epidemiology, China, 2004-2013. Emerg Infect Dis. 2013;19(11):1784-1790. doi:10.3201/eid1911.130865
6. Ying HQ, Deng QW, He BS, et al. The prognostic value of preoperative NLR, d-NLR, PLR and LMR for predicting clinical outcome in surgical colorectal cancer patients. Medical Oncology (Northwood, London, England). 2014 Dec;31(12):305. DOI: 10.1007/s12032-014-0305-0. PMID: 25355641.
7. Curbelo J, LuqueroBueno S, Galván-Román JM, et al. Inflammation biomarkers in blood as mortality predictors in community-acquired pneumonia admitted patients: Importance of comparison with neutrophil count percentage or neutrophil-lymphocyte ratio [published correction appears in PLoS One. 2019 Feb 22;14(2):e0212915]. PLoS One. 2017;12(3):e0173947. Published 2017 Mar 16. doi:10.1371/journal.pone.0173947
8. Liu X, Shen Y, Wang H, Ge Q, Fei A, et al. Prognostic Significance of Neutrophil-to-Lymphocyte Ratio in Patients with Sepsis: A Prospective Observational Study. Mediators Inflamm. 2016;2016:8191254. doi:10.1155/2016/8191254
9. Berhane M, Melku M, Amsalu A, Enawgaw B, Getaneh Z, et al. The Role of Neutrophil to Lymphocyte Count Ratio in the Differential Diagnosis of Pulmonary Tuberculosis and Bacterial Community-Acquired Pneumonia: a Cross-Sectional Study at Ayder and Mekelle Hospitals, Ethiopia. Clin Lab. 2019 Apr 1;65(4). doi: 10.7754/Clin.Lab.2018.180833. PMID: 30969087.
10. Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China [published correction appears in JAMA. 2021 Mar 16;325(11):1113]. JAMA. 2020;323(11):1061-1069. doi:10.1001/jama.2020.1585
11. Mo P, Xing Y, Xiao Y, et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China [published online ahead of print, 2020 Mar 16]. Clin Infect Dis. 2020;ciaa270. doi:10.1093/cid/ciaa270
12. Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. SeminImmunopathol. 2017;39(5):529-539. doi:10.1007/s00281-017-0629-x
13. Min, C. K., Cheon, S., Ha, N. Y., Sohn, K. M., Kim, Y., et al. (2016). Comparative and kinetic analysis of viral shedding and immunological responses in MERS patients representing a broad spectrum of disease severity. Scientific Reports, 6, [25359]. https://doi.org/10.1038/srep25359
14. Alfaraj, S. H., Al-Tawfiq, J. A., Assiri, A. Y., Alzahrani, N. A., Alanazi, A. A., & et al. (2019). Clinical predictors of mortality of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection: A cohort study. Travel Medicine and Infectious Disease. https://doi.org/10.1016/j.tmaid.2019.03.004
15. Leist SR, Jensen KL, Baric RS, Sheahan TP. Increasing the translation of mouse models of MERS coronavirus pathogenesis through kinetic hematological analysis. PLoS One. 2019;14(7):e0220126. Published 2019 Jul 24. doi:10.1371/journal.pone.0220126
16. Qin C, Zhou L, Hu Z, Zhang S, Yang S, et al. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis. 2020 Jul 28;71(15):762-768. doi: 10.1093/cid/ciaa248. PMID: 32161940; PMCID: PMC7108125.
17. Huang C, Wang Y, Li X, Ren L, Zhao J, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5. Epub 2020 Jan 24. Erratum in: Lancet. 2020 Jan 30;: PMID: 31986264; PMCID: PMC7159299.
18. Celikbilek M, Dogan S, Ozbakır O, Zararsız G, Kücük H, et al. Neutrophil-lymphocyte ratio as a predictor of disease severity in ulcerative colitis. J Clin Lab Anal. 2013 Jan;27(1):72-6. doi: 10.1002/jcla.21564. Epub 2013 Jan 4. PMID: 23292894; PMCID: PMC6807407.
19. Huang H, Wan X, Bai Y, et al. Preoperative neutrophil-lymphocyte and platelet-lymphocyte ratios as independent predictors of T stages in hilar cholangiocarcinoma. Cancer Manag Res. 2019;11:5157-5162. Published 2019 Jun 4. doi:10.2147/CMAR.S192532
20. de Jager CP, Wever PC, Gemen EF, Kusters R, van Gageldonk-Lafeber AB, et al. The neutrophil-lymphocyte count ratio in patients with community-acquired pneumonia. PLoS One. 2012;7(10):e46561. doi: 10.1371/journal.pone.0046561. Epub 2012 Oct 1. PMID: 23049706; PMCID: PMC3462173.
21. Cataudella E, Giraffa CM, Di Marca S, Pulvirenti A, Alaimo S, et al. Neutrophil-To-Lymphocyte Ratio: An Emerging Marker Predicting Prognosis in Elderly Adults with Community-Acquired Pneumonia. J Am Geriatr Soc. 2017 Aug;65(8):1796-1801. doi: 10.1111/jgs.14894. Epub 2017 Apr 13. PMID: 28407209.
22. Zheng M, Gao Y, Wang G, et al. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol Immunol. 2020;17(5):533-535. doi:10.1038/s41423-020-0402-2
23. Liu, J., Liu, Y., Xiang, P. et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med 18, 206 (2020). https://doi.org/10.1186/s12967-020-02374-0
24. Liu Y, Du X, Chen J, et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020;81(1):e6-e12. doi:10.1016/j.jinf.2020.04.002
25. Qin C, Zhou L, Hu Z, Zhang S, Yang S, et al. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis. 2020 Jul 28;71(15):762-768. doi: 10.1093/cid/ciaa248. PMID: 32161940; PMCID: PMC7108125.
26. Fu J, Kong J, Wang W, et al. The clinical implication of dynamic neutrophil to lymphocyte ratio and D-dimer in COVID-19: A retrospective study in Suzhou China. Thromb Res. 2020;192:3-8. doi:10.1016/j.thromres.2020.05.006
27. Mercier J, Voutsadakis IA. The platelets-neutrophils to lymphocytes ratio: a new prognostic marker in metastatic colorectal cancer. J Gastrointest Oncol. 2018;9(3):478-486. doi:10.21037/jgo.2018.03.13
28. Yeo AJ, Henningham A, Fantino E, et al. Increased susceptibility of airway epithelial cells from ataxia-telangiectasia to S. pneumoniae infection due to oxidative damage and impaired innate immunity [published correction appears in Sci Rep. 2020 Jul 24;10(1):12742]. Sci Rep. 2019;9(1):2627. Published 2019 Feb 22. doi:10.1038/s41598-019-38901-3
29. Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020 Jul;84:106504. doi: 10.1016/j.intimp.2020.106504. Epub 2020 Apr 13. PMID: 32304994; PMCID: PMC7152924.
30. Soylu K, Gedikli Ö, Ekşi A, Avcıoğlu Y, Soylu Aİ, et al. Neutrophil-to-lymphocyte ratio for the assessment of hospital mortality in patients with acute pulmonary embolism. Arch Med Sci. 2016 Feb 1;12(1):95-100. doi: 10.5114/aoms.2016.57585. Epub 2016 Feb 2. PMID: 26925123; PMCID: PMC4754370.
31. Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017 Jul;39(5):529-539. doi: 10.1007/s00281-017-0629-x. Epub 2017 May 2. PMID: 28466096; PMCID: PMC7079893.
32. Zeiser R, Socié G, Blazar BR. Pathogenesis of acute graft-versus-host disease: from intestinal microbiota alterations to donor T cell activation. Br J Haematol. 2016 Oct;175(2):191-207. doi: 10.1111/bjh.14295. Epub 2016 Sep 13. PMID: 27619472.
33. YangY, ShenC, LiJ, et al. Exuberant elevation of IP-10, MCP-3 and IL-1ra during SARS-CoV-2 infection is associated with disease severity and fatal outcome. MedRxiv. 2020.
34. Meo SA, Alhowikan AM, Al-Khlaiwi T, Meo IM, Halepoto DM, et al. Novel coronavirus 2019-nCoV: prevalence, biological and clinical characteristics comparison with SARS-CoV and MERS-CoV. Eur Rev Med Pharmacol Sci. 2020 Feb;24(4):2012-2019. doi: 10.26355/eurrev_202002_20379. PMID: 32141570.
35. Ren LL, Wang YM, Wu ZQ, Xiang ZC, Guo L, et al. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin Med J (Engl). 2020 May 5;133(9):1015-1024. doi: 10.1097/CM9.0000000000000722. PMID: 32004165; PMCID: PMC7147275.
36. Li Q, Guan X, Wu P, Wang X, Zhou L, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020 Mar 26;382(13):1199-1207. doi: 10.1056/NEJMoa2001316. Epub 2020 Jan 29. PMID: 31995857; PMCID: PMC7121484.
37. Chen N, Zhou M, Dong X, Qu J, Gong F, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020 Feb 15;395(10223):507-513. doi: 10.1016/S0140-6736(20)30211-7. Epub 2020 Jan 30. PMID: 32007143; PMCID: PMC7135076.
38. Ibayashi Y, Uede T, Uede T, Kikuchi K. Functional analysis of mononuclear cells infiltrating into tumors: differential cytotoxicity of mononuclear cells from tumors of immune and nonimmune rats. J Immunol. 1985 Jan;134(1):648-53. PMID: 3855260.
39. Menges T, Engel J, Welters I, Wagner RM, Little S, et al. Changes in blood lymphocyte populations after multiple trauma: association with posttraumatic complications. Crit Care Med. 1999 Apr;27(4):733-40. doi: 10.1097/00003246-199904000-00026. PMID: 10321662.
40. Wang F, Nie J, Wang H, Zhao Q, Xiong Y, et al. Characteristics of Peripheral Lymphocyte Subset Alteration in COVID-19 Pneumonia. J Infect Dis. 2020 May 11;221(11):1762-1769. doi: 10.1093/infdis/jiaa150. PMID: 32227123; PMCID: PMC7184346.
41. Bhat T, Teli S, Rijal J, Bhat H, Raza M, et al. Neutrophil to lymphocyte ratio and cardiovascular diseases: a review. Expert Rev Cardiovasc Ther. 2013 Jan;11(1):55-9. doi: 10.1586/erc.12.159. PMID: 23259445.
42. Haybar H, Pezeshki SMS, Saki N. Evaluation of complete blood count parameters in cardiovascular diseases: An early indicator of prognosis? Exp Mol Pathol. 2019 Oct;110:104267. doi: 10.1016/j.yexmp.2019.104267. Epub 2019 Jun 11. PMID: 31194963.
43. Huang Z, Fu Z, Huang W, Huang K. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: A meta-analysis. Am J Emerg Med. 2020 Mar;38(3):641-647. doi: 10.1016/j.ajem.2019.10.023. Epub 2019 Nov 18. PMID: 31785981.
44. Liu Y, Du X, Chen J, Jin Y, Peng L, et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020 Jul;81(1):e6-e12. doi: 10.1016/j.jinf.2020.04.002. Epub 2020 Apr 10. PMID: 32283162; PMCID: PMC7195072.
45. Xia X, Wen M, Zhan S, He J, Chen W. [An increased neutrophil/lymphocyte ratio is an early warning signal of severe COVID-19]. Nan Fang Yi Ke Da Xue Xue Bao. 2020 Mar 30;40(3):333-336. Chinese. doi: 10.12122/j.issn.1673-4254.2020.03.06. PMID: 32376581; PMCID: PMC7167308.
46. Liu J, Li S, Liu J, Liang B, Wang X, et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine. 2020 May;55:102763. doi: 10.1016/j.ebiom.2020.102763. Epub 2020 Apr 18. PMID: 32361250; PMCID: PMC7165294.
47. Yan Q, Li P, Ye X, Huang X, Feng B, et al. Longitudinal Peripheral Blood Transcriptional Analysis Reveals Molecular Signatures of Disease Progression in COVID-19 Patients. J Immunol. 2021 May 1;206(9):2146-2159. doi: 10.4049/jimmunol.2001325. Epub 2021 Apr 12. PMID: 33846224.
Copyright (c) 2022 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


