A Study on Acinetobacter spp isolated from various clinical samples and analysis of their susceptibility pattern at a tertiary care center
Abstract
Background: Among the gram-negative bacterial infections, Acinetobacter spp infections are ofcritical importance given the severity of infections, intrinsic resistance to most antibiotics, and alsocapability to acquire new drug resistance.
Aim: To study the prevalence of Acinetobacter spp and itsantibiotic resistance patterns in a tertiary care hospital.
Materials and methods: A retrospectivestudy, including samples from various departments, submitted to the microbiology laboratory fromJanuary 2020 to December 2020. All the samples were processed according to standardconventional methods, and the Acinetobacter isolates were studied in detail about the demographiccharacters, speciation, and antibiotic susceptibility pattern.
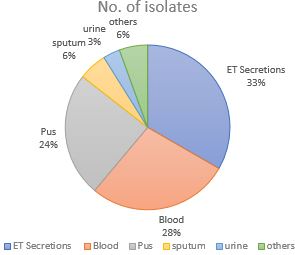
Results: Out of the 1242 positiveisolates, 7.24 % were identified as Acinetobacter species; 90% were A. baumannii. Males were mostcommon, most commonly belonging to 45-65 yrs. Out of all the recovered Acinetobacter spp, 30%were from ICU. 40% of the isolates were MDR, 74.07% from ICU and 26.98% from non-ICU settingswere statistically significant (p <0.005). Cephalosporins showed the highest resistance to theisolates Ceftazidime 82.5%, followed by Gentamicin 73.3%.
Conclusion: The present study showedthat Acinetobacter spp prevalence and antibiotic resistance (MDR) are more common in ICUs. Theemergence of carbapenem resistance in more than half the isolates is worrisome. The studysuggests susceptibility testing to be done to help select the best antimicrobial drugs for therapy,thus helping in judicial use of antibiotics is necessary to prevent the emergence of antimicrobialresistance.
Downloads
References
2. Oliveira J, Reygaert WC. Gram Negative Bacteria. [Updated 2021 Mar 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021.
3. Perry JD. A Decade of Development of Chromogenic Culture Media for Clinical Microbiology in an Era of Molecular Diagnostics. Clin Microbiol Rev. 2017 Apr;30(2):449-479.
4. Seifert, H., Baginski, R., Schulze, A. & Pulverer, G. Antimicrobial susceptibility of Acinetobacter species. Antimicrob. Agents Chemother. 1993;37(4): 750–753.
5. Agodi A, Zarilli R, Barchitta M et al. Alert surveillance of intensive care unit-acquired Acinetobacter infections in a Sicilian Hospital. Clin Microbial Infect. 2006; 12(3): 241-7.
6. Neeraj Goel, Chand Wattal, Jaswinder Kaur Oberoi, Reena Raveendran, Sanghamitra Datta, Kamal Jeet Prasad, Trend analysis of antimicrobial consumption and development of resistance in non-fermenters in a tertiary care hospital in Delhi, India, Journal of Antimicrobial Chemotherapy, 2011; 66 (7):1625–1630.
7. Rungruanghiranya S, Somboonwit C, Kanchanapoom T. Acinetobacter infection in the intensive care unit. J Infect Dis Antimicrob Agents. 2005; 22(2): 77-9.
8. Collee JG, Fraser AG, Marmion BP, Simmons A. 14th ed. New York: Churchill-Livingstone; Mackie and McCartney Practical Medical Microbiology. 1999
9. CLSI. Performance standards for antimicrobial disc susceptibility testsing. 30th ed. CLSI supplement M-100 Wayne, PA: Clinical and Lab Standards Institute; 2020.
10. Dent LL, Marshall DR, Pratap S, Hulette RB. Multidrug resistant Acinetobacter baumannii: a descriptive study in a city hospital. BMC Infect Dis. 2010 Jul 7;10:196. doi: 10.1186/1471-2334-10-196. PMID: 20609238; PMCID: PMC2909240.
11. Uwingabiye J, Lemnouer A, Roca I, Alouane T, Frikh M, Belefquih B, Bssaibis F, Maleb A, Benlahlou Y, Kassouati J, Doghmi N, Bait A, Haimeur C, Louzi L, Ibrahimi A, Vila J, Elouennass M. Clonal diversity and detection of carbapenem resistance encoding genes among multidrug-resistant Acinetobacter baumannii isolates recovered from patients and environment in two intensive care units in a Moroccan hospital. Antimicrob Resist Infect Control. 2017 Sep 26;6:99. doi: 10.1186/s13756-017-0262-4. PMID: 28959441; PMCID: PMC5615474.
12. Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K. EPIC II Group of Investigators.International Study of the Prevalence and Outcomes of Infection in Intensive Care Units. JAMA. 2009;302(21):2323-2329.
13. Sharma RK, Mamoria VP. A Prospective Study on Prevalence and Antibiotic Susceptibility Pattern of Acinetobacter baumannii in Clinical Samples obtained from Patients admitted in Various Wards and Intensive Care Units. J Mahatma Gandhi Univ Med Sci Tech 2017;2(3):122-127.
14. Rajkumari S, Pradhan S, Sharma D, Jha B. Prevalence and Antibiogram of Acinetobacter Species Isolated from Various Clinical Samples in a Tertiary Care Hospital. Journal of College of Medical Sciences-Nepal. 2020 Mar 31;16(1):26-32.
15. Kaur R, Kaur S, Oberoi L, Singh K, Nagpal N, Kaur M. Prevalence & antimicrobial profile of acinetobacter Spp. isolated from tertiary care hospital. International Journal of Contemporary Medical Research 2021;8(2):B1-B6.
16. Lone R, Shah A, Kadri SM, Lone S, Faisal S. Nosocomial Multi-Drug-Resistant Acinetobacter Infections- Clinical Findings, Risk Factors and Demographic Characteristics. Bangladesh J Med Microbiol. 2009;3:34-8.
17. Joshi SG, Litake GM, Niphadkar KB, Ghole VS. Multidrug resistant Acinetobacter baumannii isolates from a teaching hospital. J Infect Chemother. 2003 Jun;9(2):187-90. doi: 10.1007/s10156-002-0224-4. PMID: 12872781
18. Nageeb W, Kamel M, Zakaria S, Metwally L. Phenotypic characterization of Acinetobacter baumannii isolates from intensive care units at a tertiary-care hospital in Egypt. EMHJ-Eastern Mediterranean Health Journal. 2014; 20 ( 3): 203-211.
19. Ayenew Z, Tigabu E, Syoum E, Ebrahim S, Assefa D, Tsige E. Multidrug resistance pattern of Acinetobacter species isolated from clinical specimens referred to the Ethiopian Public Health Institute: 2014 to 2018 trend anaylsis. Plos one. 2021 Apr 29;16(4):e0250896.
20. Punpanich W, Nithitamsakun N, Treeratweeraphong V, Suntarattiwong P.Risk factors for carbapenem nonsusceptibility and mortality in Acinetobacter baumannii bacteremia in children. Int J Infect Dis. 2012;16(11):e811- e815.
21. García-Garmendia JL, Ortiz-Leyba C, Garnacho-Montero J, Jiménez-Jiménez FJ, Pérez-Paredes C, Barrero-Almodóvar AE, Gili-Miner M. Risk Factors for Acinetobacter baumannii Nosocomial Bacteremia in Critically Ill Patients:a Cohort Study. Clin Infect Dis. 2001; 33(7):939–46.
22. Xia Y, Lu C, Zhao J, Han G, Chen Y, Wang F, Yi B, Jiang G, Hu X, Du X, Wang Z, Lei H, Han X, Han L. A bronchofiberoscopy-associated outbreak of multidrug-resistant Acinetobacter baumannii in an intensive care unit in Beijing, China. BMC Infect Dis. 2012 Dec 3;12:335. doi: 10.1186/1471-2334-12-335. PMID: 23198973; PMCID: PMC3562511.
23. Tahseen U, Talib MT. Acinetobacter infections as an emerging threat in intensive care units. J Ayub Med Coll Abbottabad 2015 Jan-Mar;27(1):113-116
24. Saha S, Devi KM, Damrolien S, Devi KS. A study of Acinetobacter infections in a tertiary care hospital in Northeast India. Int J Res Med Sci 2018;6(6):2076-80.
25. Taneja N, Singh G, Singh M, Sharma M. Emergence of tigecycline & colistin resistant Acinetobacter baumanii in patients with complicated urinary tract infections in north India. Indian J Med Res. 2011 Jun;133(6):681-4. PMID: 21727671; PMCID: PMC3136000..
26. De Francesco MA, Ravizzola G, Peroni L, Bonfanti C, Manca N. Prevalence of multidrug-resistant Acinetobacter baumannii and Pseudomonas aeruginosa in an Italian hospital. Journal of infection and public health. 2013 Jun 1;6(3):179-85.
27. Shareek, P. S., Sureshkumar, D., Ramgopalakrishnan, Ramasubramanian, V., Ghafur, K. A. & Thirunarayanan, M. A. (2012). Antibiotic Sensitivity Pattern of Blood Isolates of Acinetobacter Species in a Tertiary Care Hospital: A Retrospective Analysis. American Journal of Infectious Diseases, 8(1), 65-69. https://doi.org/10.3844/ajidsp.2012.65.69.
28. Dash M, Padhi S, Mohanty I et al. Frequency, risk factors and Antibiogram of Acinetobacter species isolated from various clinical samples in a tertiary care hospital in Odhisa, India. Avicenna J Med. 2013; 3(4):97-102.
29. Almaghrabi MK, Joseph MR, Assiry MM, Hamid ME. Multidrug-resistant Acinetobacter baumannii: an emerging health threat in Aseer Region, Kingdom of Saudi Arabia. Canadian Journal of Infectious Diseases and Medical Microbiology, 2018; 2018. https://doi.org/10.1155/2018/9182747 PMID: 29623140
30. Rebic V, Masic N, Teskeredzic S, Aljicevic M, Abduzaimovic A, Rebic D. The importance of Acinetobacter species in the hospital environment. Medical Archives, 2018; 72(5):325.
31. Raina D, Sharma N, Mahawal BS, Khanduri A, Pandita A. Speciation and antibiotic resistance pattern of Acinetobacter species in a tertiary care hospital in Uttarakhand. International Journal of Medical Research & Health Sciences 2016; 5(4): 89-96
Copyright (c) 2022 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


