Relationship between blood group and risk of infection, intubation and death in Covid pandemic
Abstract
Background: Few people infected by the coronavirus become seriously ill, while others show mild symptoms or are asymptomatic. Recent research points out that the ABO blood group might play an essential role in a person’s susceptibility and severity of COVID-19 infection.
Aims: This study is conducted to find the relationship between ABO groups and COVID-19 infection.
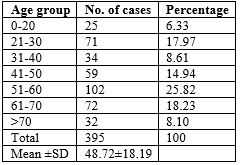
Methods: A total of 395 patients were included in this study. The study population was divided based on ABO blood groups into types A+, A−, B+, B −, AB, O+, and O−.
Results: Blood group B was associated with high susceptibility to infection. We found slightly increased infection prevalence among the Rh factor positive blood group. The risk of infection was decreased among blood groups with Rh factor negative. Cases having blood group B have higher chances of covid-19 infection followed by AB and type O.
Conclusion: We estimated Rh-negative blood types to have a protective effect for covid -19 infection. Our results add to the growing body of evidence suggesting blood group type may play a role in COVID-19 infection.
Downloads
References
Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020 Feb 15;395(10223):470-473. doi: 10.1016/S0140-6736(20)30185-9.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5.
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020 Feb 20;382(8):727-733. doi: 10.1056/NEJMoa2001017.
Anon. WHO Director-General’s opening remarks at the media briefing on COVID-19—11 March 2020.
Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020 Apr 16;181(2):281-292.e6. doi: 10.1016/j.cell.2020.02.058.
Coronavirus disease 2019 (COVID-19) Weekly Epidemiological Update 1 World Health Organization WHO Coronavirus disease 2019 Weekly Epidemiological Updates (2020-08-17)
Sajadi MM, Habibzadeh P, Vintzileos A, Shokouhi S, Miralles-Wilhelm F, Amoroso A. Temperature, Humidity, and Latitude Analysis to Estimate Potential Spread and Seasonality of Coronavirus Disease 2019 (COVID-19). JAMA Netw Open. 2020 Jun 1;3(6):e2011834. doi: 10.1001/jamanetworkopen.2020.11834.
Scafetta N. Distribution of the SARS-CoV-2 Pandemic and Its Monthly Forecast Based on Seasonal Climate Patterns. Int J Environ Res Public Health. 2020 May 17;17(10):3493. doi: 10.3390/ijerph17103493.
Kershaw KN, Diez Roux AV, Carnethon M, Darwin C, Goff DC Jr, Post W, et al. Geographic variation in hypertension prevalence among blacks and whites: the multi-ethnic study of atherosclerosis. Am J Hypertens. 2010 Jan;23(1):46-53. doi: 10.1038/ajh.2009.211.
Samouda H, Ruiz-Castell M, Bocquet V, Kuemmerle A, Chioti A, Dadoun F, et al. Geographical variation of overweight, obesity and related risk factors: Findings from the European Health Examination Survey in Luxembourg, 2013-2015. PLoS One. 2018 Jun 14;13(6):e0197021. doi: 10.1371/journal.pone.0197021.
Cheng Y, Cheng G, Chui CH, Lau FY, Chan PK, Ng MH, et al. ABO blood group and susceptibility to severe acute respiratory syndrome. JAMA. 2005 Mar 23;293(12):1450-1. doi: 10.1001/jama.293.12.1450-c.
Hutson AM, Atmar RL, Graham DY, Estes MK. Norwalk virus infection and disease is associated with ABO histo-blood group type. J Infect Dis. 2002 May 1;185(9):1335-7. doi: 10.1086/339883.
Yamamoto F, Cid E, Yamamoto M, Blancher A. ABO research in the modern era of genomics. Transfus Med Rev. 2012 Apr;26(2):103-18. doi: 10.1016/j.tmrv.2011.08.002.
Zhao J, Yang Y, Huang H, Li D, Gu D, Lu X, et al. Relationship Between the ABO Blood Group and the Coronavirus Disease 2019 (COVID-19) Susceptibility. Clin Infect Dis. 2021 Jul 15;73(2):328-331. doi: 10.1093/cid/ciaa1150.
Guillon P, Clément M, Sébille V, Rivain JG, Chou CF, Ruvoën-Clouet N, et al. Inhibition of the interaction between the SARS-CoV spike protein and its cellular receptor by anti-histo-blood group antibodies. Glycobiology. 2008 Dec;18(12):1085-93. doi: 10.1093/glycob/cwn093.
Breiman A, Ruvën-Clouet N, Le Pendu J. Harnessing the natural anti-glycan immune response to limit the transmission of enveloped viruses such as SARS-CoV-2. PLoS Pathog. 2020 May 21;16(5):e1008556. doi: 10.1371/journal.ppat.1008556.
Chung CM, Wang RY, Chen JW, Fann CS, Leu HB, Ho HY, et al. A genome-wide association study identifies new loci for ACE activity: potential implications for response to ACE inhibitor. Pharmacogenomics J. 2010 Dec;10(6):537-44. doi: 10.1038/tpj.2009.70.
Guillon P, Clément M, Sébille V, Rivain JG, Chou CF, Ruvoën-Clouet N, et al. Inhibition of the interaction between the SARS-CoV spike protein and its cellular receptor by anti-histo-blood group antibodies. Glycobiology. 2008 Dec;18(12):1085-93. doi: 10.1093/glycob/cwn093.
Zhao J, Yang Y, Huang H, Li D, Gu D, Lu X, et al. Relationship Between the ABO Blood Group and the Coronavirus Disease 2019 (COVID-19) Susceptibility. Clin Infect Dis. 2021 Jul 15;73(2):328-331. doi: 10.1093/cid/ciaa1150.
Göker H, Aladağ Karakulak E, Demiroğlu H, Ayaz Ceylan ÇM, Büyükaşik Y, Inkaya AÇ, et al. The effects of blood group types on the risk of COVID-19 infection and its clinical outcome. Turk J Med Sci. 2020 Jun 23;50(4):679-683. doi: 10.3906/sag-2005-395.
Dai X. ABO blood group predisposes to COVID-19 severity and cardiovascular diseases. Eur J Prev Cardiol. 2020 Sep;27(13):1436-1437. doi: 10.1177/2047487320922370.
van Vark LC, Bertrand M, Akkerhuis KM, Brugts JJ, Fox K, Mourad JJ, et al. Angiotensin-converting enzyme inhibitors reduce mortality in hypertension: a meta-analysis of randomized clinical trials of renin-angiotensin-aldosterone system inhibitors involving 158,998 patients. Eur Heart J. 2012 Aug;33(16):2088-97. doi: 10.1093/eurheartj/ehs075.
Hessami A, Shamshirian A, Heydari K, Pourali F, Alizadeh-Navaei R, Moosazadeh M, et al. Cardiovascular diseases burden in COVID-19: Systematic review and meta-analysis. Am J Emerg Med. 2021 Aug;46:382-391. doi: 10.1016/j.ajem.2020.10.022.
Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect. 2020 Aug;81(2):e16-e25. doi: 10.1016/j.jinf.2020.04.021.
Arend P. How blood group A might be a risk and blood group O be protected from coronavirus (COVID-19) infections (how the virus invades the human body via ABO(H) blood group–determining carbohydrates). Availableat:.10August2020.https://figshare.com/articles/preprint/How_blood_group_O_could_be_protected_from_Coronavirus_Covid-19_infections/12019035.
Preece AF, Strahan KM, Devitt J, Yamamoto F, Gustafsson K. Expression of ABO or related antigenic carbohydrates on viral envelopes leads to neutralization in the presence of serum containing specific natural antibodies and complement. Blood. 2002 Apr 1;99(7):2477-82. doi: 10.1182/blood.v99.7.2477.
Mattos, Luiz C. de, and Haroldo W. Moreira. "Genetic of the ABO blood system and its link with the immune system." Revista Brasileira de Hematologia e Hemoterapia 26.1 (2004): 60-63.
Cheng Y, Cheng G, Chui CH, Lau FY, Chan PK, Ng MH, et al. ABO blood group and susceptibility to severe acute respiratory syndrome. JAMA. 2005 Mar 23;293(12):1450-1. doi: 10.1001/jama.293.12.1450-c.
Zhao, J., et al. "X., Wang, PG (2020). Relationship between the ABO blood group and the COVID-19 susceptibility." MedRxiv.
Severe Covid-19 GWAS Group, Ellinghaus D, Degenhardt F, Bujanda L, Buti M, Albillos A, et al. Genomewide Association Study of Severe Covid-19 with Respiratory Failure. N Engl J Med. 2020 Oct 15;383(16):1522-1534. doi: 10.1056/NEJMoa2020283.
Copyright (c) 2022 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


