Risk factors and microbiological features of surgical site infections
Abstract
Background: Surgical site infections are the infections of the tissues, organs or spaces exposed by surgeons during the performance of an invasive procedure manifested in the postoperative period within 30 days after a surgical procedure and up to one year if an implant was placed in the patient. SSI is still higher in India as compared to western data leading to increased morbidity and mortality. This study aimed to analyse the factors associated with SSI and its microflora in a tertiary care centre.
Methods: A descriptive cross-sectional study was done for one year in a tertiary care centre in Bareilly, U.P. All the patients who underwent surgeries related to git pathology in the surgery department, either emergency or elective with surgical site infections, were included in this study. Patients less than 18, all cases operated else were, or re-operated were excluded from this study. All traumatic abdominal surgeries were also excluded from this study.
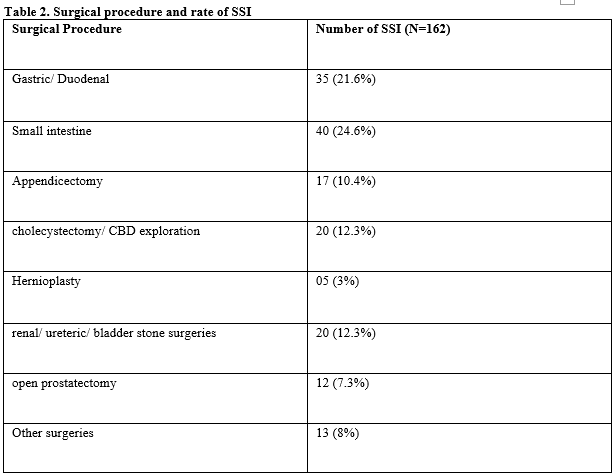
Results: The present study revealed SSI was associated with 82 (9.4%) cases among elective and 80 (21%) in emergency surgeries. Superficial incision SSI was found to be most common (90 cases), followed by deep incisional SSI (60 patients) and organ/space SSI (12 cases). Minor intestine surgeries were most commonly associated with SSI. The microbiological organism most widely isolated was E. Coli (41.2%), followed by Staphylococcus aureus (27.5%), Klebsiella (16.5%), group A beta-haemolytic Streptococci (9.1%) and Pseudomonas (5.5%).
Conclusions: Surgical site infection still causes considerable morbidity and high cost to the health care system and is becoming increasingly crucial in medico-legal aspects. Prevention of SSI requires a targeted approach to improve health care workers' knowledge, practising the guidelines strictly regarding asepsis and optimising the patient before surgery. Reduction in rate of SSI will improve cosmesis and make the results of operations better as a whole.
Downloads
References
National Nosocomial infection Survillance (NNIS) System. National Nosocomial infection Surveillance (NNIS) report, data summary from October 1986-April 1996, issued May 1996. A report from the National Nosocomial infection Surveillance (NNIS) System. Am J Infect Control. 1996 Oct.24(5):380-8 [Medline].
Ganguly, P. S., Md Yunus Khan, and Abida Malik. Nosocomial infections and hospital procedures. Indian Journal of Community Medicine 25.1 (2000): 39.
Owens CD, Stoessel K. Surgical site infections: epidemiology, microbiology and prevention. J Hosp Infect. 2008 Nov;70 Suppl 2:3-10. doi: 10.1016/S0195-6701(08)60017-1.
Nichols RL. Preventing surgical site infections: a surgeon's perspective. Emerg Infect Dis. 2001 Mar-Apr;7(2):220-4. doi: 10.3201/eid0702.010214.
Martone WJ, Nichols RL. Recognition, prevention, surveillance, and management of surgical site infections: introduction to the problem and symposium overview. Clin Infect Dis. 2001 Sep 1;33 Suppl 2:S67-8. doi: 10.1086/321859.
Kobayashi, M., Mohri, Y., Inoue, Y., Okita, Y., Miki, C., & Kusunoki, M. Continuous follow-up of surgical site infections for 30 days after colorectal surgery. World journal of surgery, 32.6 (2008): 1142-1146.
Blumetti, J., Luu, M., Sarosi, G., Hartless, K., McFarlin, J., et al. Surgical site infections after colorectal surgery: do risk factors vary depending on the type of infection considered?. Surgery, 142.5 (2007): 704-711.
Konishi, T., Watanabe, T., Kishimoto, J., & Nagawa, H. Elective colon and rectal surgery differ in risk factors for wound infection: results of prospective surveillance. Annals of surgery, 244.5 (2006): 758.
Bennett SN, McNeil MM, Bland LA, Arduino MJ, Villarino ME, Perrotta DM, et al. Postoperative infections traced to contamination of an intravenous anesthetic, propofol. N Engl J Med. 1995 Jul 20;333(3):147-54. doi: 10.1056/NEJM199507203330303.
Nichols RL, Smith JW. Bacterial contamination of an anesthetic agent. N Engl J Med. 1995 Jul 20;333(3):184-5. doi: 10.1056/NEJM199507203330310.
Nichols RL. Prevention of infection in high risk gastrointestinal surgery. Am J Med. 1984 May 15;76(5A):111-9. doi: 10.1016/0002-9343(84)90252-3.
Lubega A, Joel B, Justina Lucy N. Incidence and Etiology of Surgical Site Infections among Emergency Postoperative Patients in Mbarara Regional Referral Hospital, South Western Uganda. Surg Res Pract. 2017;2017:6365172. doi: 10.1155/2017/6365172.
Giri S, Kandel BP, Pant S, Lakhey PJ, Singh YP, Vaidya P. Risk factors for surgical site infections in abdominal surgery: a study in Nepal. Surg Infect (Larchmt). 2013 Jun;14(3):313-8. doi: 10.1089/sur.2012.108.
Ikeanyi UO, Chukwuka CN, Chukwuanukwu TO. Risk factors for surgical site infections following clean orthopaedic operations. Niger J Clin Pract. 2013 Oct-Dec;16(4):443-7. doi: 10.4103/1119-3077.116886.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


