Serum adiponectin among different stages of type 2 diabetes mellitus patients
Abstract
Background: Type 2 diabetes mellitus is a chronic metabolic disorder that leads to micro and macrovascular complications. Nephropathy is the most common microvascular complication. For diagnosis of nephropathy in T2DM patients by using urinary albumin, this is not a sensitive and specific biomarker because it is elevated in other conditions. we aimed to evaluate the serum adiponectin for early detection of nephropathy in patients with type 2 diabetes mellitus.
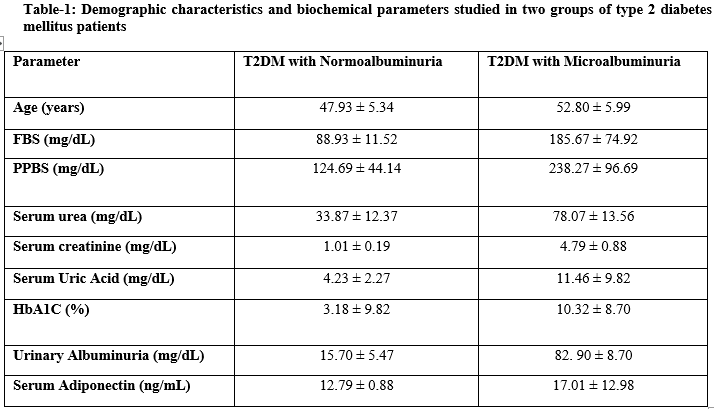
Methods: A total of 60 subjects were included in the present study and further subdivided into 30 patients T2DM with normoalbuminuria, 30 patients with microalbuminuria. All the patients were included after obtaining institutional ethical permission and consent forms. Blood and urine samples were collected from all the subjects and proceed with further analysis. Appropriate statistical analyses were used for different types of data analysis.
Results: Increased levels of FBS, PPBS, HbA1C and serum adiponectin were observed in two groups of T2DM patients. Statistically elevated levels of serum Urea, Creatinine and Uric acid levels were observed in patients T2DM with microalbuminuria when compared to T2DM with normoalbuminuria. The serum adiponectin was positively correlated with FBS, PPBS, HbA1C, Urea, Creatinine, Uric Acid and Urinary Albumin in patients with two groups of T2DM.
Conclusion: This study concluded that measuring the serum adiponectin levels may be useful for the early detection of nephropathy in patients with T2DM.
Downloads
References
Stumvoll M, Goldstein BJ, van Haeften TW. Type 2 diabetes: principles of pathogenesis and therapy. Lancet. 2005 Apr 9-15;365(9467):1333-46. doi: 10.1016/S0140-6736(05)61032-X.
American Diabetes Association. Erratum. Classification and diagnosis of diabetes. Sec. 2. In Standards of Medical Care in Diabetes-2016. Diabetes Care 2016;39(Suppl. 1):S13-S22. Diabetes Care. 2016 Sep;39(9):1653. doi: 10.2337/dc16-er09.
Frier BM. Diabetes mellitus, 20 th ed. In: Boon A Colledge R. Davidson’s Principles and practice of medicine, Churchill Living stone, 2006:805-48.
Gosmanov AR, Gosmanova EO, Dillard-Cannon E. Management of adult diabetic ketoacidosis. Diabetes Metab Syndr Obes. 2014 Jun 30;7:255-64. doi: 10.2147/DMSO.S50516.
Fowler, Michael J. "Microvascular and macrovascular complications of diabetes." Clinical diabetes 26.2 (2008): 77-82.
Ruggenenti P, Remuzzi G. Nephropathy of type 1 and type 2 diabetes: diverse pathophysiology, same treatment? Nephrol Dial Transplant. 2000 Dec;15(12):1900-2. doi: 10.1093/ndt/15.12.1900.
Fukami K, Yamagishi S, Ueda S, Okuda S. Role of AGEs in diabetic nephropathy. Curr Pharm Des. 2008;14(10):946-52. doi: 10.2174/138161208784139710.
Tziomalos K, Athyros VG. Diabetic Nephropathy: New Risk Factors and Improvements in Diagnosis. Rev Diabet Stud. 2015 Spring-Summer;12(1-2):110-8. doi: 10.1900/RDS.2015.12.110.
Cao Z, Cooper ME. Pathogenesis of diabetic nephropathy. J Diabetes Investig. 2011 Aug 2;2(4):243-7. doi: 10.1111/j.2040-1124.2011.00131.x.
Mezzano S, Aros C, Droguett A, Burgos ME, Ardiles L, Flores C, et al. NF-kappaB activation and overexpression of regulated genes in human diabetic nephropathy. Nephrol Dial Transplant. 2004 Oct;19(10):2505-12. doi: 10.1093/ndt/gfh207.
Dasu MR, Devaraj S, Park S, Jialal I. Increased toll-like receptor (TLR) activation and TLR ligands in recently diagnosed type 2 diabetic subjects. Diabetes Care. 2010 Apr;33(4):861-8. doi: 10.2337/dc09-1799.
Basi S, Fesler P, Mimran A, Lewis JB. Microalbuminuria in type 2 diabetes and hypertension: a marker, treatment target, or innocent bystander? Diabetes Care. 2008 Feb;31 Suppl 2:S194-201. doi: 10.2337/dc08-s249.
Sun Y, Xun K, Wang C, Zhao H, Bi H, Chen X, Wang Y. Adiponectin, an unlocking adipocytokine. Cardiovasc Ther. 2009 Spring;27(1):59-75. doi: 10.1111/j.1755-5922.2008.00069.x.
Robinson K, Prins J, Venkatesh B. Clinical review: adiponectin biology and its role in inflammation and critical illness. Crit Care. 2011 Apr 20;15(2):221. doi: 10.1186/cc10021.
Wang ZV, Scherer PE. Adiponectin, the past two decades. J Mol Cell Biol. 2016 Apr;8(2):93-100. doi: 10.1093/jmcb/mjw011. Epub 2016 Mar 18.
Sharma K, Ramachandrarao S, Qiu G, Usui HK, Zhu Y, Dunn SR, et al. Adiponectin regulates albuminuria and podocyte function in mice. J Clin Invest. 2008 May;118(5):1645-56. doi: 10.1172/JCI32691.
Rutkowski JM, Wang ZV, Park AS, Zhang J, Zhang D, Hu MC, et al. Adiponectin promotes functional recovery after podocyte ablation. J Am Soc Nephrol. 2013 Feb;24(2):268-82. doi: 10.1681/ASN.2012040414.
de Boer IH, Sibley SD, Kestenbaum B, Sampson JN, Young B, Cleary PA, et al. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study Research Group. Central obesity, incident microalbuminuria, and change in creatinine clearance in the epidemiology of diabetes interventions and complications study. J Am Soc Nephrol. 2007 Jan;18(1):235-43. doi: 10.1681/ASN.2006040394.
de Boer IH, Rue TC, Cleary PA, Lachin JM, Molitch ME, Steffes MW, et al. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study Research Group, White NH, Danis RP, Davis MD, Hainsworth D, Hubbard LD, Nathan DM. Long-term renal outcomes of patients with type 1 diabetes mellitus and microalbuminuria: an analysis of the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications cohort. Arch Intern Med. 2011 Mar 14;171(5):412-20. doi: 10.1001/archinternmed.2011.16.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998 Sep 12;352(9131):837-53.
Timothy C. Evans, Peter C. Diabetic Nephropathy. Clinical Diabetes. 2000;18:7-46.
Fukami K, Yamagishi S, Ueda S, Okuda S. Role of AGEs in diabetic nephropathy. Curr Pharm Des. 2008;14(10):946-52. doi: 10.2174/138161208784139710.
Tziomalos K, Athyros VG. Diabetic Nephropathy: New Risk Factors and Improvements in Diagnosis. Rev Diabet Stud. 2015 Spring-Summer;12(1-2):110-8. doi: 10.1900/RDS.2015.12.110.
Cao Z, Cooper ME. Pathogenesis of diabetic nephropathy. J Diabetes Investig. 2011 Aug 2;2(4):243-7. doi: 10.1111/j.2040-1124.2011.00131.x.
Mezzano S, Aros C, Droguett A, Burgos ME, Ardiles L, Flores C, et al. NF-kappaB activation and overexpression of regulated genes in human diabetic nephropathy. Nephrol Dial Transplant. 2004 Oct;19(10):2505-12. doi: 10.1093/ndt/gfh207.
Dasu MR, Devaraj S, Park S, Jialal I. Increased toll-like receptor (TLR) activation and TLR ligands in recently diagnosed type 2 diabetic subjects. Diabetes Care. 2010 Apr;33(4):861-8. doi: 10.2337/dc09-1799.
Basi S, Fesler P, Mimran A, Lewis JB. Microalbuminuria in type 2 diabetes and hypertension: a marker, treatment target, or innocent bystander? Diabetes Care. 2008 Feb;31 Suppl 2:S194-201. doi: 10.2337/dc08-s249.
Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes. 2003 Jan;52(1):102-10. doi: 10.2337/diabetes.52.1.102.
Leahy JL, Hirsch IB, Peterson KA, Schneider D. Targeting beta-cell function early in the course of therapy for type 2 diabetes mellitus. J Clin Endocrinol Metab. 2010 Sep;95(9):4206-16. doi: 10.1210/jc.2010-0668.
Widjaja A, Stratton IM, Horn R, Holman RR, Turner R, Brabant G. UKPDS 20: plasma leptin, obesity, and plasma insulin in type 2 diabetic subjects. J Clin Endocrinol Metab. 1997 Feb;82(2):654-7. doi: 10.1210/jcem.82.2.3744.
Kopecký J, Flachs P, Bardová K, Brauner P, Prazák T, Sponarová J. Modulation of lipid metabolism by energy status of adipocytes: implications for insulin sensitivity. Ann N Y Acad Sci. 2002 Jun;967:88-101.doi: 10.1111/j.1749-6632.2002.tb04267.x.
Okutan H, Ozcelik N, Yilmaz HR, Uz E. Effects of caffeic acid phenethyl ester on lipid peroxidation and antioxidant enzymes in diabetic rat heart. Clin Biochem. 2005 Feb;38(2):191-6. doi: 10.1016/j.clinbiochem.2004.10.003.
Park K, Gross M, Lee DH, Holvoet P, Himes JH, Shikany JM, et al. Oxidative stress and insulin resistance: the coronary artery risk development in young adults study. Diabetes Care. 2009 Jul;32(7):1302-7. doi: 10.2337/dc09-0259.
Ouedraogo R, Wu X, Xu SQ, Fuchsel L, Motoshima H, Mahadev K, et al. Adiponectin suppression of high-glucose-induced reactive oxygen species in vascular endothelial cells: evidence for involvement of a cAMP signaling pathway. Diabetes. 2006 Jun;55(6):1840-6. doi: 10.2337/db05-1174.
Yamauchi T, Kamon J, Ito Y, Tsuchida A, Yokomizo T, Kita S, etal. Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature. 2003 Jun 12;423(6941):762-9. doi: 10.1038/nature01705.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


