Relationship of Neutrophil Lymphocyte Ratio (NLR) with Parathyroid Hormone (PTH) in Maintenance Hemodialysis Patients
Abstract
Background: Neutrophil-Lymphocyte-Ratio (NLR), a simple derived parameter of routine Complete Blood Counts (CBC), has been shown to be better than WBC count as a marker for inflammation in many contexts. Inflammation is associated with adverse outcomes in hemodialysis patients.
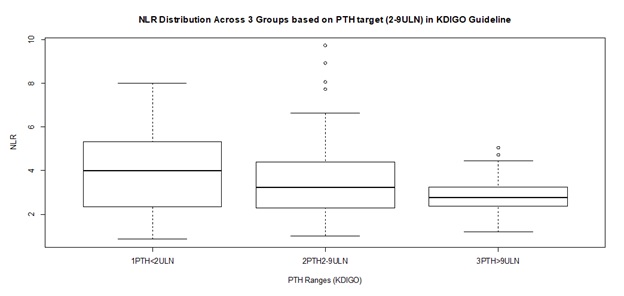
Methods: A cross sectional study was designed on 100 maintenance hemodialysis Patients in a tertiary care hospital in Eastern India after IRB permission and informed consent. 88 complete results became available. Complete blood count (CBC), routine PTH and biochemistry analysis were performed. KDIGO 2009 cut offs were used to classify patients by PTH levels (PTH<2ULN, PTH 2-9ULN & PTH>9 ULN). NLR was calculated and NLR of 3.5 was used as high inflammation cut off.
Results: In Analysis of 88 samples, significant Pearson Correlation with NLR was shown by Albumin, Hemoglobin, PTH, Gender, Age, and Sugar, but involved collinearities. Multiple Linear Regression with Robust estimation of Standard Errors retained only PTH as a significant predictor (Beta= -0.273, P=0.033) of NLR and Albumin as a borderline significant predictor (Beta= -0.501, P= 0.061). The population was partitioned into 3 sets based on PTH as per KDIGO guideline.
Conclusion: Our study suggests that PTH is a significant predictor of inflammation as measured by NLR, independent of the other parameters, and it has an overall weak negative association with inflammation especially in the mid-range (PTH 2-9 ULN) subgroup, which largely corroborates with available but scant literature.
Downloads
References
. Levin, A., Tonelli, M., Bonventre, J., Coresh, J., Donner, J.-A., Fogo, A. B., Fox, C. S., Gansevoort, R. T., Heerspink, H. J. L., Jardine, M., Kasiske, B., Köttgen, A., Kretzler, M., Levey, A. S., Luyckx, V. A., Mehta, R., Moe, O., Obrador, G., Pannu, N., … ISN Global Kidney Health Summit participants. (2017). Global kidney health 2017 and beyond: A roadmap for closing gaps in care, research, and policy. Lancet (London, England), 390(10105), 1888–1917. https://doi.org/10.1016/S0140-6736(17)30788-2
Bikbov, B., Purcell, C. A., Levey, A. S., Smith, M., Abdoli, A., Abebe, M., Adebayo, O. M., Afarideh, M., Agarwal, S. K., Agudelo-Botero, M., Ahmadian, E., Al-Aly, Z., Alipour, V., Almasi-Hashiani, A., Al-Raddadi, R. M., Alvis-Guzman, N., Amini, S., Andrei, T., Andrei, C. L., … Vos, T. (2020). Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 395(10225), 709–733. https://doi.org/10.1016/S0140-6736(20)30045-3
Bharati, J., & Jha, V. (2020). Global Dialysis Perspective: India. Kidney360, 1(10), 1143–1147. https://doi.org/10.34067/KID.0003982020
Couser, W. G., Remuzzi, G., Mendis, S., & Tonelli, M. (2011). The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney International, 80(12), 1258–1270.
Achinger, S. G., & Ayus, J. C. (2013). Inflammation from dialysis, can it be removed? Nephrology Dialysis Transplantation, 28(4), 770–773. https://doi.org/10.1093/ndt/gfs480
Cobo, G., Lindholm, B., & Stenvinkel, P. (2018). Chronic inflammation in end-stage renal disease and dialysis. Nephrology Dialysis Transplantation, 33(Suppl 3), iii35–iii40. https://doi.org/10.1093/ndt/gfy175
Li, H., Lu, X., Xiong, R., & Wang, S. (2017). High neutrophil-to-lymphocyte ratio predicts cardiovascular mortality in chronic hemodialysis patients. Mediators of Inflammation, 2017.
Catabay, C., Obi, Y., Streja, E., Soohoo, M., Park, C., Rhee, C. M., Kovesdy, C. P., Hamano, T., & Kalantar-Zadeh, K. (2017). Lymphocyte Cell Ratios and Mortality among Incident Hemodialysis Patients. American Journal of Nephrology, 46(5), 408–416. https://doi.org/10.1159/000484177
Zhao, W.-M., Tao, S.-M., & Liu, G.-L. (2020). Neutrophil-to-lymphocyte ratio in relation to the risk of all-cause mortality and cardiovascular events in patients with chronic kidney disease: A systematic review and meta-analysis. Renal Failure, 42(1), 1059–1066. https://doi.org/10.1080/0886022X.2020.1832521
Li, X., Zhang, X., Yang, Y., Du, L., Zhang, J., Zhang, Y., & Wang, C. (2019). Increased neutrophil/leukocyte ratio of the peripheral blood in chronic heart failure patients with renal dysfunction. INTERNATIONAL JOURNAL OF CLINICAL AND EXPERIMENTAL MEDICINE, 12(5), 5951–5959.
Ouellet, G., Malhotra, R., Penne, E. L., Usvya, L., Levin, N. W., & Kotanko, P. (2016). Neutrophil-lymphocyte ratio as a novel predictor of survival in chronic hemodialysis patients. Clinical Nephrology, 85(4), 191–198.
Malhotra, R., Marcelli, D., von Gersdorff, G., Grassmann, A., Schaller, M., Bayh, I., Scatizzi, L., Etter, M., Guinsburg, A., & Barth, C. (2015). Relationship of neutrophil-to-lymphocyte ratio and serum albumin levels with C-reactive protein in hemodialysis patients: Results from 2 international cohort studies. Nephron, 130(4), 263–270.
Solak, Y., Yilmaz, M. I., Sonmez, A., Saglam, M., Cakir, E., Unal, H. U., Gok, M., Caglar, K., Oguz, Y., Yenicesu, M., Karaman, M., Ay, S. A., Gaipov, A., Turk, S., Vural, A., & Carrero, J. J. (2013). Neutrophil to lymphocyte ratio independently predicts cardiovascular events in patients with chronic kidney disease. Clinical and Experimental Nephrology, 17(4), 532–540. https://doi.org/10.1007/s10157-012-0728-x
Moe, S. M. (n.d.). Definition and classification of renal osteodystrophy and chronic kidney disease–mineral bone disorder (CKD–MBD). In The Spectrum of Mineral and Bone Disorders in Chronic Kidney Disease. Oxford University Press. Retrieved January 12, 2021, from https://oxfordmedicine.com/view/10.1093/med/9780199559176.001.1/med-9780199559176-chapter-001
Cavalier, E., Carlisi, A., Bekaert, A.-C., Rousselle, O., Chapelle, J.-P., & Delanaye, P. (2012). New insights on the stability of the parathyroid hormone as assayed by an automated 3rd generation PTH assay. Clinica Chimica Acta; International Journal of Clinical Chemistry, 413(1–2), 353–354. https://doi.org/10.1016/j.cca.2011.09.034
Rafieian-Kopaei, M., Baradaran, A., & Nasri, H. (2012). Association of secondary hyperparathyroidism with malnutrition and inflammation in maintenance hemodialysis patients. Life Science Journal, 9(3), 1871–1878.
Jaqueto, M., Delfino, V. D. A., Bortolasci, C. C., Barbosa, D. S., Morimoto, H. K., Frange, R. F. N., Ferreira, L. F. F., Guimarães, F. B. dos S., Jaqueto, M., Delfino, V. D. A., Bortolasci, C. C., Barbosa, D. S., Morimoto, H. K., Frange, R. F. N., Ferreira, L. F. F., & Guimarães, F. B. dos S. (2016). Are PTH levels related to oxidative stress and inflammation in chronic kidney disease patients on hemodialysis? Brazilian Journal of Nephrology, 38(3), 288–295. https://doi.org/10.5935/0101-2800.20160045
Christensen, M. H. E., Fenne, I. S., Nordbø, Y., Varhaug, J. E., Nygård, K. O., Lien, E. A., & Mellgren, G. (2015). Novel inflammatory biomarkers in primary hyperparathyroidism. European Journal of Endocrinology, 173(1), 9–17. https://doi.org/10.1530/EJE-14-1038
Dukkipati, R., Kovesdy, C. P., Colman, S., Budoff, M. J., Nissenson, A. R., Sprague, S. M., Kopple, J. D., & Kalantar-Zadeh, K. (2010). Association of relatively low serum parathyroid hormone with malnutrition-inflammation complex and survival in maintenance hemodialysis patients. Journal of Renal Nutrition, 20(4), 243–254. https://doi.org/10.1053/j.jrn.2009.10.006
Toraman, A., Aras, F., Hekimsoy, Z., & Kursat, S. (2019). IS THERE A RELATIONSHIP BETWEEN PARATHYROID HORMONE AND NEUTROPHIL LYMPHOCYTE RATIO OR PLATELET LYMPHOCYTE RATIO? Acta Endocrinologica (Bucharest), 15(1), 96–101. https://doi.org/10.4183/aeb.2019.96
Emam, A. A., Mousa, S. G., Ahmed, K. Y., & Al-Azab, A. A. (2012). Inflammatory Biomarkers in Patients with Asymptomatic Primary Hyperparathyroidism. Medical Principles and Practice, 21(3), 249–253. https://doi.org/10.1159/000334588
Cheng, S.-P., Liu, C.-L., Liu, T.-P., Hsu, Y.-C., & Lee, J.-J. (2014). Association between parathyroid hormone levels and inflammatory markers among US adults. Mediators of Inflammation, 2014, 709024. https://doi.org/10.1155/2014/709024
Venkatesan, S., Chakkarai, K., Arulvijayavani, S., Senthilkumar, G. P., Manikandan, R., & Kalyaperumal, M. (2017). Association between vitamin D, parathyroid hormone and inflammatory markers in urolithiasis patients. Journal of Renal Injury Prevention, 6(4), 240–243. https://doi.org/10.15171/jrip.2017.45
Yang, Y., Da, J., Yi, J., Yuan, J., & Zha, Y. (2020). Low serum parathyroid hormone is a risk factor for peritonitis episodes in incident peritoneal dialysis patients: A retrospective study. https://doi.org/10.21203/rs.3.rs-55536/v2
Otawa, M., Tanoue, R., Kido, H., Sawa, Y., & Yamashita, J. (2015). Intermittent administration of parathyroid hormone ameliorates periapical lesions in mice. Journal of Endodontics, 41(5), 646–651. https://doi.org/10.1016/j.joen.2014.12.008
Stutz, C., Batool, F., Petit, C., Strub, M., Kuchler-Bopp, S., Benkirane-Jessel, N., & Huck, O. (2020). Influence of parathyroid hormone on periodontal healing in animal models: A systematic review. Archives of Oral Biology, 120, 104932. https://doi.org/10.1016/j.archoralbio.2020.104932
Hong, Y. A., Kim, J. H., Kim, Y. K., Chang, Y. K., Park, C. W., Kim, S. Y., Kim, Y. S., Kang, S.-W., Kim, N.-H., Kim, Y.-L., & Yang, C. W. (2020). Low parathyroid hormone level predicts infection-related mortality in incident dialysis patients: A prospective cohort study. The Korean Journal of Internal Medicine, 35(1), 160–170. https://doi.org/10.3904/kjim.2018.264
Feroze, U., Molnar, M. Z., Dukkipati, R., Kovesdy, C. P., & Kalantar-Zadeh, K. (2011). Insights Into Nutritional and Inflammatory Aspects of Low Parathyroid Hormone in Dialysis Patients. Journal of Renal Nutrition, 21(1), 100–104. https://doi.org/10.1053/j.jrn.2010.10.006
Geara, A. S., Castellanos, M. R., Bassil, C., Schuller-Levis, G., Park, E., Smith, M., Goldman, M., & Elsayegh, S. (2010). Effects of Parathyroid Hormone on Immune Function. Clinical and Developmental Immunology, 2010. https://doi.org/10.1155/2010/418695
Perry, H. M., Chappel, J. C., Bellorin-Font, E., Tamao, J., Martin, K. J., & Teitelbaum, S. L. (1984). Parathyroid hormone receptors in circulating human mononuclear leukocytes. The Journal of Biological Chemistry, 259(9), 5531–5535.
Clementi, G., Caruso, A., Cutuli, V., Prato, A., Fiore, C. E., & Amico-Roxas, M. (1992). Parathyroid hormone fragment 1-34 and anti-inflammatory effect. Archives Internationales De Pharmacodynamie Et De Therapie, 315, 87–95.
Nielsen, P. K., Rasmussen, AAK, Butters, R., Feldt-Rasmussen, U., Bendtzen, K., Diaz, R., Brown, Em., & Olgaard, K. (1997). Inhibition of PTH Secretion by Interleukin-1β in Bovine Parathyroid Glandsin VitroIs Associated with an Up-Regulation of the Calcium-Sensing Receptor mRNA. Biochemical and Biophysical Research Communications, 238(3), 880–885. https://doi.org/10.1006/bbrc.1997.7207
McCauley, L. K., Dalli, J., Koh, A. J., Chiang, N., & Serhan, C. N. (2014). Cutting edge: Parathyroid hormone facilitates macrophage efferocytosis in bone marrow via proresolving mediators resolvin D1 and resolvin D2. Journal of Immunology (Baltimore, Md.: 1950), 193(1), 26–29. https://doi.org/10.4049/jimmunol.1301945
Iamartino, L., Elajnaf, T., Kallay, E., & Schepelmann, M. (2018). Calcium-sensing receptor in colorectal inflammation and cancer: Current insights and future perspectives. World Journal of Gastroenterology, 24(36), 4119–4131. https://doi.org/10.3748/wjg.v24.i36.4119
Caruso, A., Amico-Roxas, M., Cutuli, V., Prato, A., Fiore, C. E., & Clementi, G. (1991). Parathyroid hormone fragment 1-34 inhibits drug-induced inflammation in various experimental models. European Journal of Pharmacology, 198(1), 85–88. https://doi.org/10.1016/0014-2999(91)90565-8
Platas, J., Guillén, M. I., Gomar, F., Castejón, M. A., Esbrit, P., & Alcaraz, M. J. (2017). Anti-senescence and Anti-inflammatory Effects of the C-terminal Moiety of PTHrP Peptides in OA Osteoblasts. The Journals of Gerontology: Series A, 72(5), 624–631. https://doi.org/10.1093/gerona/glw100
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


