Inducible Clindamycin Resistance in Staphylococcus aureus isolated from pus samples in an Orthopaedic tertiary care centre.
Abstract
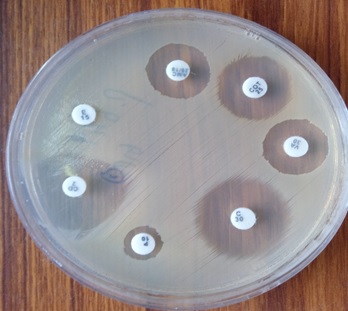
Introduction: Clindamycin is a commonly used antibiotic to treat skin and soft tissue infections caused by Staphylococcus aureus particularly Methicillin-Resistant Staphylococcus aureus (MRSA) infection. In vitro routine tests for clindamycin susceptibility may fail to detect inducible clindamycin resistance due to genes resulting in treatment failure, thus necessitating the need to detect such resistance by a simple D - test on a routine basis.
Materials and Methods: 165 isolates of Staphylococcus aureus were subjected to routine antibiotic susceptibility testing including Oxacillin (1µg) and Cefoxitin (30µg) by Kirby Bauer disc diffusion method. Inducible clindamycin resistance was detected by D test as per CLSI guidelines on erythromycin resistant isolates.
Results: 24 (14.5%) isolates showed inducible clindamycin resistance, 8 (4.84%) showed constitutive resistance while the remaining 59 (35.75%) showed MS phenotype. Inducible clindamycin resistance and MS phenotype were found higher in MRSA (21.42%, 40.47%) as compared to MSSA (7.40%, 30.86%).
Conclusion: This study showed that the D test should be used as a mandatory method in routine disc diffusion testing to detect inducible clindamycin resistance.
Downloads
References
Yilmaz G, Aydin K, Iskender S, Caylan R, Koksal I. Detection and prevalence of inducible clindamycin resistance in staphylococci. J Med Microbiol.2007; 56:104-106.
Deotale V, Mendiratta DK, Raut U, Narang P . Inducible Clindamycin resistance in Staphylococcus aureus isolated from clinical samples. Indian J Med Microbiol.2010; 28: 124-126.
Upadhya A, Biradar S. Prevalence of inducible clindamycin resistance in Staphylococcus aureus in a tertiary care hospital in north-east Karnataka, India. Int Health Sci Int J .2011;1:21-24.
Banik A, Khyriem A B, Gurung J, Lyngdoh V W. Inducible and constitutive clindamycin resistance in Staphylococcus aureus in a northeastern Indian tertiary care hospital. J Infect Dev Ctries 2015;9(7):725-731
Juyal D, Shamanth A, Pal S, Sharma M, Prakash R, Sharma N. The prevalence of inducible clindamycin resistance among Staphylococci in a tertiary care hospital – A Study from the Garhwal Hills of Uttarakhand, India. J Clin Diagn Res.2013; 7:61-65
Gadepalli R, Dhawan B, Mohanty S, Kapil A, Das BK, Chaudhry R. Inducible clindamycin resistance in clinical isolates of Staphylococcus aureus.Indian J Med Res.2006; 123:571-573.
Steward CD, Raney PM, Morell AK, Williams PP, McDougal LK, Jevitt L, et al. Testing for induction of clindamycin resistance inj erythromycin resistant isolates of Staphylococcus aureus. J Clin Microbiol 2005; 43:1716-1721.
Fiebelkorn KR, Crawford SA, McElmeel ML, Jorgensen JH. Practical disc diffusion method for detection of inducible clindamycin resistance in Staphylococcus aureus and coagulase-negative Staphylococci. J Clin Microbiol 2003; 41:4740-4744.
Clinical and laboratory standards institute. Performance standards for antimicrobial susceptibility testing; 13th ed. CLSI standard M02. Wayne, PA: Clinical Laboratory Standards Institute; 2018
Kloos WE, Banerman TL. Staphylococcus and Micrococcus, Chapter 22. In: Manual of clinical microbiology. 7th ed Murray PR, Baron EJ, Pfaller MA, Tenover FC, Yolken RH, Editors. Washington DC: ASM Press;1999.p.264-82
Ajantha G, Kulkarni R, Shetty J, Shubhada C, Jain P.Phenotypic detection of inducible clindamycin resistance among Staphylococcus aureus isolates by using the lower limit of recommended inter-disc distance. Indian J Pathol Microbiol. 2008; 51: 376-378
Patel M, Waites KB, Moser SA, Cloud GA, Hoesley CJ.Prevalence of inducible clindamycin resistance among Community and Hospital associated Staphylococcus aureus Isolates. J Clin Microbiol. 2006; 44:2481-2484.
Lavallee C, Rouleau D, Gaudreau C, Roger M, Tsimiklis C, Locas MC, Gagnon S, Delorme J, Labbe AC. Performance of an Agar Dilution Method and a Vitek 2 card for detection of Inducible clindamycin resistance in Staphylococcus spp. J Clin Microbiol 2010; 48:1354-1357
Singh T, Deshmukh AB, Chitnis V, Bajpal T. Inducible clindamycin resistance among Staphylococcus aureus isolates in a tertiary care hospital. Int J Health Allied Sci 2016;5:111-114
Rahabar M, Hajia M. Inducible clindamycin resistance in Staphylococcus aureus: A cross-sectional report. Pak J Biol Sci 2007; 10:189-192
Prabhu K, Rao S, Rao V. Inducible clindamycin resistance in Staphylococcus aureus isolated from clinical samples. J Lab Physicians.2011 Jan-Jun;3(10):25-27
Schreckenberger PC, Ilendo E, Ristow KL. Incidence of Constitutive and Inducible clindamycin resistance in Staphylococcus aureus and coagulase negative staphylococcus in a community and a tertiary care hospital. J Clin Microbiol.2004;42: 2777-2779
Levin TP, Suh B, Axelrod P, Trunat AL, Fekete T. Potential clindamycin resistance in clindamycin- susceptible, erythromycin- resistant Staphylococcus aureus. Report of a clinical failure. Antimicrob Agents Chemother. 2005;49:1222-4
Rao GG. Should clindamycin be used in the treatment of patients with infections caused by erythromycin resistant Staphylococci? J Antimicrob Chemother 2000; 45:715
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


