Study of Neutrophil-Lymphocyte ratio (NLR) in diabetes mellitus
Abstract
Introduction: Diabetes mellitus is a systemic disease having serious microvascular complications. Neutrophil-lymphocyte ratio (NLR) provides insight about subclinical inflammation and thus acts as a prognostic marker for diabetes mellitus and it's vascular complications.
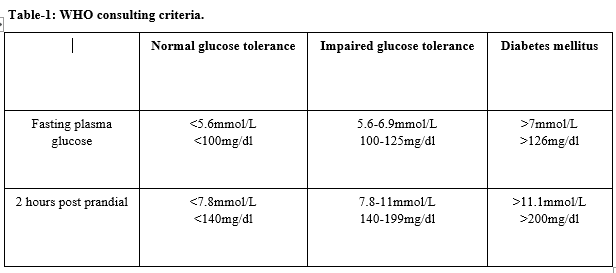
Aim: To study the relationship between neutrophil-lymphocyte ratio with different grades of glucose intolerance. Materials and Methods Cases for the present study include known cases of diabetes mellitus and normal subjects from KR hospital, Mysuru. Fasting blood glucose (FBS) and postprandial blood glucose (PPBS) of study subjects are taken into account to grade glucose intolerance under three categories- Normal glucose tolerance, Impaired glucose tolerance, and diabetes mellitus. Neutrophil-lymphocyte ratios are calculated and compared with blood glucose levels.
Results: NLR showed no significant variation in different grades of glucose intolerance. NLR was increased in patients with neuropathy, glaucoma, and blurring of vision when compared with those patients without any complication.
Conclusion: NLR is increased in subjects having diabetes mellitus with complications when compared to the subjects with diabetes mellitus under control. Hence NLR can be considered as an early and prognostic marker for microvascular complications in patients with diabetes mellitus.
Downloads
References
Shiny A, Bibin Y S, Shanthirani C S, Regin B S, Anjana R A, Balasubramanyam M, et al. Association of neutrophil-lymphocyte ratio with glucose intolerance: an indicator of systemic inflammation in patients with type 2 diabetes. Diabetes Technol Ther. 2014;16(8):524-530. doi: https://doi.org/10.1089/dia.2013.0264.
Akash MSH, Rehman K, Chen S. Role of inflammatory mechanisms in pathogenesis of type 2 diabetes mellitus. J. Cell. Biochem. 2013;114(3):525-531. doi: https://doi.org/10.1002/jcb.24402.
Okyay G U, Inal S, Onec K, Er R E, Pasaoglu O, Pasaoglu H et al. Neutrophil to lymphocyte ratio in evaluation of inflammation in patients with chronic kidney disease. Renal Fail. 2012;35(1):29-36. doi: https://doi.org/10.3109/0886022x.2012.734429.
Khandare SA, Chittawar S, Nahar N, Dubey TN, Qureshi Z. Study of neutrophil-lymphocyte ratio as novel marker for diabetic nephropathy in type 2 diabetes. Indian J Endocr Metab. 2017;21(3):387-392. Available from: http://www.ijem.in/text.asp?2017/21/3/387/205486.
Xu T, Weng Z, Pei C, Yu S, Chen Y, Guo W et al. The relationship between neutrophil-to-lymphocyte ratio and diabetic peripheral neuropathy in type 2 diabetes mellitus. Medicine 2017;96(45):e8289. doi: https://doi.org/10.1097/md.0000000000008289.
Azab B, Daoud J, Naeem FB, et al. Neutrophil-to-lymphocyte ratio as a predictor of worsening renal function in diabetic patients (3 year follow-up study). Ren Fail. 2012;34(5):571-576. https://doi.org/10.3109/0886022x.2012.668741.
Huang W, Haung J, Liu QLin F, He Z, Zeng Z et al. Neutrophil- Lymphocyte ratio a reliable predictive marker of early stage diabetic nephropathy. Clin Endocrinol. 2015;82(2):229-233. doi: https://doi.org/10.1111/cen.12576.
Wang RT, Zhang JR, Li Y, Liu T, Yu KJ. Neutrophil lymphocyte ratio is associated with arterial stiffness in diabetic retinopathy in type 2 diabetes complications. J Diabetes Complications 2015;29(2):245-249. doi: https://doi.org/10.1016/j.jdiacomp.2014.11.006.
Kahraman C, Yumun G, Kahraman NK, Namdar ND, Cosgun S. Neutrophil lymphocyte ratio in diabetes mellitus patients with and without diabetic foot ulcer. Eur J Med Sci.2014;1:8-13.
Azab B, Daoud J, Naeem FB, Nasr R, Ross J, Ghimire P, et al. Neutrophil-to-lymphocyte ratio as a predictor of worsening renal function in diabetes patients (3 year follow-up study). Ren Fail. 2012;34(5):571-576. doi: https://doi.org/10.3109/0886022X.2012.668741.
Barnes PJ, Karin M. Nuclear factor- kappa B: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med. 1997;336(15):1066-1071. doi: https://doi.org/10.1056/nejm199704103361506.
Kawamura N, Dyck PJ, Schmeichel AM, Engelstad JK, Low PA, Dyck PJ. Inflammatory mediators in diabetic and non-diabetic lumbosacral radiculoplexus neuropathy. Acta Neuropathol. 2008;115(2):231-239. doi: https://doi.org/10.1007/s00401-007-0326-2.
Gokulakrishnan K, Deepa R, Sampathkumar R, Balasubramanyam M, Mohan V. Association of leukocyte count with varying degrees of glucose intolerance in Asian Indians: the Chennai Urban Rural Epidemiology Study (Cures-26). Metab Syndr Relat Disord. 2009:7(3):205-210. doi: https://doi.org/10.1089/met.2008.0024.
Lum H, Roebuck KA: Oxidant stress and endothelial cell disfunction. Am J Physiol Cell Physiol. 2001;280(4):C719-C741. doi: https://doi.org/10.1152/ajpcell.2001.280.4.c719.
Vincet AM, Callaghan BC, Smith AL, Feldman EL. Diabetic neuropathy: cellular mechanisms as therapeutic targets. Nat Rev Neurol. 2011;7(10):573-583. doi: https://doi.org/10.1038/nrneurol.2011.137.
Kampoli AM, Tousoulis D, Briasoulis A, Latsios G, Papageorgiou N, Stefanadis C. Potential pathogenic inflammatory mechanisms of endothelial dysfunction induced by type 2 diabetes mellitus. Curr Pharm Des. 2011;17(37):4147-4158. doi: https://doi.org/10.2174/138161211798764825.
Uceyler N, Rogausch JP, Tokyo KV, Sommer C. Differential expression of cytokines in painful and painless neuropathies. Neurology. 2007;69(1):42-49. doi: https://doi.org/10.1212/01.wnl.0000265062.92340.a5.
Doupis J, Lyons TE, Wu S, Charalambos Gnardellis, Dinh T, Veves A et al. Microvascular reactivity and inflammatory cytokines in painful and painless peripheral diabetic neuropathy. J Clin Endocrinol Metab. 2009;94(6):215-263. doi: https://doi.org/10.1210/jc.2008-2385.
Ulu SM, Dogan M, Ahsen A, Altug A, Demir K, Acarturk G, et al. Neutrophil-to-lymphocyte ratio as a quick and reliable predictive marker to diagnose the severity of diabetic retinopathy. Diabetes Technol Ther. 2013;15(11):942-947. doi: https://doi.org/10.1089/dia.2013.0097.
Ulu S, Bucak A, Ulu MS, Ahsen A, Duran A, Yucedag F, et al. Neutrophil-lymphocyte ratio as anew predictive and prognostic factor at the hearing loss of diabetic patients. Eur Arch Otorhinolaryngol. 2014;271(10):2681-2686. doi: https://doi.org/10.1007/s00405-013-2734-3.
Ozturk ZA, Kuyumcu ME, Yesil Y, Savas E, Yildiz H, Kepekci Y, et al. Is There a link between neutrophil-lymphocyte ratio and microvascular complications in geriatric diabetic patients. J Endocrinol Invest. 2013;36(8):593-599. doi: https://doi.org/10.3275/8894.
Okyay GU, Inal S, Onec K, Er RE, Pasaoglu O, Pasaoglu H, et al. Neutrophil to lymphocyte ratio in evaluation of inflammation in patients wuth chronic kidney disease. Ren Fail. 2013;35(1):29-36. doi: https://doi.org/10.3109/0886022x.2012.734429.
Akbas EM, Demirtas L, Ozcicek A, Timuroglu A, Bakirci EM, Hamur H, et al. Association of epicardial adipose tissue, neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio with diabetic nephropathy. Int J Clin Exp Med. 2014;7(7):1794-801
Zouridakis E, Avanzas P, Arroyo-Espliguero R, Fredericks S, Kaski JC. Markers of inflammation and rapid coronary artery disease progression in patients with stable angina pectoris. Circulation. 2004;110(13):1747-1753. doi: https://doi.org/10.1161/01.cir.0000142664.18739.92.
Hussain M, Babar M Z B, Akhtar L, Hussain M S. Neutrophil lymphocyte ratio (NLR): A well assessment tool of glycemic control in type-2 diabetic patients. Pak J Med Sci. 2017;33(6):6,1366-1370. doi: https://doi.org/10.12669/pjms.336.12900.
Chung K-P, Chang H-T, Lo S-C, Chang L-Y, Lin S-Y, Cheng A, et al. Severe lymphopenia is associated with elevated plasma interleukin-15 levels and increased mortality during severe sepsis. Shock.2015;43(6):569-575. doi: https://doi.org/10.1097/shk.0000000000000347.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


