Study of drug resistance pattern among isolated strains of Mycobacterium tuberculosis against individual antimycobacterial drugs
Abstract
Background: In the laboratory in-vitro antimycobacterial sensitivity testing is done conventionally by exposing the test strain to individual drugs by one of the recommended methods. Thus the present work was planned to assess the effects of various antimycobacterial drugs individually.
Methods: The study included 73 strains of Mycobacterium tuberculosis isolated from 216 patients suffering from pulmonary tuberculosis and who visited the hospital for the first time and who had not received any antimycobacterial chemotherapy. From all these patients early morning spot sample was collected in a wide-mouthed sterile container and transported immediately to the laboratory.
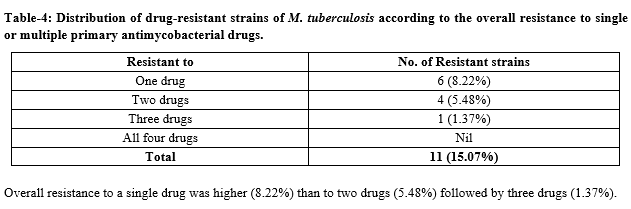
Result: Out of 73 stains, 62 (84.93%) were sensitive to all primary antimycobacterial agents and 11 (15.07%) were resistant to one or more drugs. 6 (8.22%) were resistant to Isoniazid (INH), 9 (12.33%) and 2 (2.74%) strains were resistant to Rifampicin (R’cin) and Streptomycin respectively. Overall resistance to a single drug was higher (8.22%) than to two drugs (5.48%) followed by three drugs (1.37%).
Conclusion: Treatment of tuberculosis with appropriate drugs for a defined period is an important factor in the complete remission of disease in the individual patient, as well as in the management of the disease in a community.
Downloads
References
World Health Organization. Global tuberculosis control: epidemiology, strategy, financing: WHO report 2009. World Health Organization; 2009.
Espinal MA, Laszlo A, Simonsen L, Boulahbal F, Kim SJ, Reniero A, et al. Global trends in resistance to anti tuberculosis drugs. N Engl J Med. 2001;344 (17):1294-1303. doi: https://doi.org/10.1056/nejm200104263441706.
Mitichson DA. Drug resistance in mycobacteria. Br Med Bull. 1984;40(1):84-90. doi: https://doi.org/10.1093/oxfordjournals.bmb.a071952.
Paramasivan CN. An overview on drug resistant tuberculosis in India. Lung India.1998;16(1):21-28.
Gopi PG, Vallishayee RS, Appe Gowda BN, Paramasivan CN, Ranganatha S, Venkataramu KV, Phaniraj BS et.al. A tuberculosis prevalence survey based on symptoms questioning and sputum examinations. Ind J Tub 1998;44(4):171-180.
Cohn DL, Bustreo F, Raviglione MC. Drug resistant tuberculosis: Review of the worldwide situations and SHO/IUATLD global surveillance project. Clin Infect Dis. 1997;24(1):121-130. doi: https://doi.org/10.1093/clinids/24.supplement_1.s121.
WHO (2002), Global Tuberculosis Control, Surveillance Planning, Financing, WHO Report 2002. Available at https://apps.who.int/iris/bitstream/handle/10665/42889/9241562641.pdf?sequence=2.
Government. of India (2002), Annual Report 2001-2002, DGHS, New Delhi.
Lwanga, Stephen Kaggwa, Lemeshow, Stanley and World Health Organization. Sample size determination in health studies : a practical manual / S. K. Lwanga and S. Lemeshow. World Health Organization.1991. Available at https://apps.who.int/iris/handle/10665/40062.
Macki and McCarney’s Practical Medical Microbiology. 13th Ed, Practical Med Microbiol. 1985;2:399.
Manual for laboratory technician. Revised National Tuberculosis Control Programme (RNTCP) DGHS, New Delhi (May 1999).
Paramasivan CN, Bhaskaran K, Venkataraman P, Chandrasekaran V, Narayanan PR. Surveillance of drug resistance in tuberculosis in the state of Tamil Nadu. Indian Journal of Tuberculosis. 2000;47(1):27-33.
Tuberculosis research center [ICMR]. Chemotherapy of drug resistant tuberculosis: The tuberculosis research center experience over 40 years. Ind J Tub. 2000;47:201.
Koch A. Vareldzis B. Styblo K. Multidrug-resistant tuberculosis and its control. Res Microbiol. 1993;144(2):104-110. doi: https://doi.org/10.1016/0923-2508(93)90023-u.
World Health Organization. Laboratory evaluation of drug resistant tuberculosis. Document WHO/TB/93. 171. Geneva, World Health Organization, 1993. Available at https://apps.who.int/iris/bitstream/handle/10665/62460/WHO_TB_93.171.pdf.
Kim S, Hong Y. Drug resistance of Mycobacterium tuberculosis in Korea. Tubercle and Lung Dis. 1992; 73(4):219-224. doi: https://doi.org/10.1016/0962-8479(92)90090-7.
Chaulet P, Boulahbal F. Clinical Trial of a Combination of Three Drugs in Fixed Proportions in the Treatment of Tuberculosis. Groupe De Travail Sur La Chimiothérapie De La Tuberculose. Tuber Lung Dis. 1995;76(5):407-412. doi: https://doi.org/10.1016/0962-8479(95)90006-3.
Jain NK, Chopra KK, Prasad G. Initial and acquired Isoniazid and Rifampicin resistance to M. tuberculosis and its implications for treatment. Ind J Tub. 1992;39(2):121-124.
Singh M. Tuberculosis: Triumph and Tragedy. J Indian Med Assoc. 2003;101(3):190.
Neville K, Bromberg A, Bromberg R, Bonk S, Hanna BA, Rom WN. The third epidemic—multidrug-resistant tuberculosis. Chest. 1994;105(1):45-48. doi: https://doi.org/10.1378/chest.105.1.45.
Chawla PK. Klapper PJ, Kamholz SL, Pollack AH, Heurich AE. Drug resistant tuberculosis in an urban population including patients at risk for human immunodeficiency virus infection. Am Rev Respir Dis. 1992;146(2):280-284. doi: https://doi.org/10.1164/ajrccm/146.2.280.
Trivedi SS, Desai SG. Primary anti-tuberculosis drug resistance and acquired Rifampicin resistance in Gujarat India Tubercle. 1988;69(1):37-42. doi: https://doi.org/10.1016/0041-3879(88)90038-4.
Vasanthakumari R, Jagannath K, Rajasekarn S. Bacteriological status and prevalence of drug resistance in district tuberculosis centers in Tamil Nadu. Lung India.1993;11(1-2):27-31.
Sophia V. Balasangameshwara VH, Jagannatha PS, Kumar P. Initial drug resistance among tuberculosis patients under DOTS programme in Bangalore City. Ind J Tub. 2004;51:17-21
Jindal SK. Drug resistance Tuberculosis India – Clinical approach. Ind J Tub. 1995; 42:233.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


