Analysis of antibiotic usage for surgical prophylaxis in a tertiary care hospital in Bangalore, Karnataka, India
Abstract
Introduction: Appropriately administered antibiotic prophylaxis reduces the incidence of surgical wound infection. The timing of antibiotic administration is very critical. The first dose should always be given before the procedure, preferably within 60 minutes before incision. Re-administration at one to two half-lives of the antibiotic is recommended for the duration of the procedure. In general, postoperative administration is not recommended except for cardiothoracic surgeries.
Materials and Methods: This is a retrospective study done over a period of 6 months from January 2019 to June 2019 in a tertiary care hospital in Bangalore. A continuous 100 patients who underwent an elective surgery were audited regarding the antibiotic indication, choice, dosage, dosing interval, and timing of first antibiotic administration prior to skin incision and duration of prophylaxis were compared with the CDC guideline recommendations and hospital antibiotic policy.
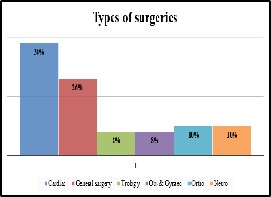
Results: A total of 100 surgeries were audited. Out of this, 4% were clean 84% were clean contaminated 4% were contaminated and 8% were dirty. The most commonly used antibiotics were cephalosporins 74% aminoglycosides 36%, β lactams 14%, and fluoroquinolones 2%. The three parameters tested for adherence showed individual compliance of 92% for appropriate selection of antibiotics, 85% for the appropriate administration, and 56% for the appropriate duration of antibiotics, respectively.
Conclusion: The results highlight the challenges of disseminating evidence-based protocols systematically into routine clinical practice. Various measures are needed to improve appropriateness of prescriptions and adherence include the development of evidence-based guidelines in collaboration with surgeons, increased outcome-based research to document benefits of appropriate antibiotic use, continuing education to disseminate information to practitioners etc.
Downloads
References
Shapiro M. Prophylaxis in otolaryngologic surgery and neurosurgery: a critical review. Rev Infect Dis. 1991;13(10):S858-S868. doi: https://doi.org/10.1093/clinids/13.supplement_10.s858.
Friberg D, Lundberg C. Antibiotic prophylaxis in major head and neck surgery when clean-contaminated wounds are established. Scand J Infect Dis. 1990;70:87-90.
Haines SJ. Efficacy of antibiotic prophylaxis in clean neurosurgical operations. Neurosurgery. 1989;24(3):401-405. doi: https://doi.org/10.1227/00006123-198903000-00016.
Aznar R, Mateu M, Miro JM, Gatell JM, Gimferrer JM, Aznar E, et al. Antibiotic prophylaxis in non-cardiac thoracic surgery: cefazolin versus placebo. Eur J Cardiothorac Surg. 1991;5(10):515-518. doi: https://doi.org/10.1016/1010-7940(91)90103-q.
Ilves R, Cooper JD, Todd TR, Pearson FG. Prospective, randomized, double-blind study using prophylactic cephalothin for major, elective, general thoracic operations. J Thorac Cardiovasc Surg. 1981;81(6):813-817.
Doebbeling BN, Pfaller MA, Kuhns KR, Massanari RM, Behrendt DM, Wenzel RP. Cardiovascular surgery prophylaxis. A randomized, controlled comparison of cefazolin and cefuroxime. J Thorac Cardiovasc Surg. 1990;99(6):981-989.
Ariano RE, Zhanel GG. Antimicrobial prophylaxis in coronary bypass surgery: a critical appraisal. DICP. 1991;25(5):478-484. doi: https://doi.org/10.1177/106002809102500508.
Kaiser AB, Herrington JL Jr, Jacobs JK, Mulherin JL Jr, Roach AC, Sawyers JL. Cefoxitin versus erythromycin, neomycin, and cefazolin in colorectal operations. Importance of the duration of the surgical procedure. Ann Surg. 1983;198(4):525-530. doi: https://dx.doi.org/10.1097%2F00000658-198310000-00012.
Clarke JS, Condon RE, Bartlett JG, Gorbach SL, Nichols RL, Ochi S. Preoperative oral antibiotics reduce septic complications of colon operations: results of prospective, randomized, double-blind clinical study. Ann Surg. 1977;186(3):251-259. doi: https://doi.org/10.1097/00000658-197709000-00003.
Baum ML, Anish DS, Chalmers TC, Sacks HS, Smith H Jr, Fagerstrom RM. A survey of clinical trials of antibiotic prophylaxis in colon surgery: evidence against further use of no-treatment controls. N Engl J Med. 1981;305(14):795-799. doi: https://doi.org/10.1056/nejm198110013051404.
Stellato TA, Danziger LH, Gordon N, Hau T, Hull CC, Zollinger RM Jr, et al. Antibiotics in elective colon surgery. A randomized trial of oral, systemic, and oral/systemic antibiotics for prophylaxis. Am Surg. 1990;56(4):251-254.
Solla JA, Rothenberger DA. Preoperative bowel preparation. A survey of colon and rectal surgeons. Dis Colon Rectum. 1990;33(2):154-159. doi: https://doi.org/10.1007/bf02055549.
Hemsell DL. Prophylactic antibiotics in gynecologic and obstetric surgery. Rev Infect Dis. 1991;13(10):S821-S841. doi: https://doi.org/10.1093/clinids/13.supplement_10.s821.
Pitt HA, Postier RG, MacGowan AW, Frank LW, Surmak AJ, Sitzman JV, et al. Prophylactic antibiotics in vascular surgery. Topical, systemic, or both? Ann Surg. 1980;192(3):356-364. doi: https://doi.org/10.1097/00000658-198009000-00011.
Kaiser AB, Clayson KR, Mulherin JL Jr, Roach AC, Allen TR, Edwards WH, et al. Antibiotic prophylaxis in vascular surgery. Ann Surg. 1978;188(3):283-289. doi: https://doi.org/10.1097/00000658-197809000-00003.
Platt R, Zucker JR, Zaleznik DF, Hopkins CC, Dellinger EP, Karchmer AW, et al. Prophylaxis against wound infection following herniorrhaphy or breast surgery. J Infect Dis. 1992;166(3):556-560. doi: https://doi.org/10.1093/infdis/166.3.556.
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152(8):784-791. doi: https://doi.org/10.1001/jamasurg.2017.0904.
Allegranzi B, Bischoff P, de Jonge S, Kubilay NZ, Zayed B, Gomes SM, et al. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16(12):e276-e287. doi: https://doi.org/10.1016/S1473-3099(16)30398-X.
Sampol-Manos E, Leone M, Karouia D, Savelli V, Ragni E, Rossi D, et al. Prophylaxis with ciprofloxacin for open prostatectomy: comparison of tissue penetration with two oral doses. J Chemother. 2006;18(2):225-226. doi: https://doi.org/10.1179/joc.2006.18.2.225.
Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect. 2013;14(1):73-156. doi: https://doi.org/10.1089/sur.2013.9999.
Weber WP, Mujagic E, Zwahlen M, Bundi M, Hoffmann H, Soysal SD, et al. Timing of surgical antimicrobial prophylaxis: a phase 3 randomised controlled trial. Lancet Infect Dis. 2017;17(6):605-614. doi: https://doi.org/10.1016/s1473-3099(17)30176-7.
Tissingh EK, Sudlow A, Jones A, Nolan JF. Orthopaedic surgical site infection surveillance in NHS England: national audit of current practice. Bone Joint J. 2017;99-B(2):171-174. doi: https://doi.org/10.1302/0301-620X.99B2.BJJ-2016-0420.R1.
Singh S, Davies J, Sabou S, et al. Challenges in reporting surgical site infections to the national surgical site infection surveillance and suggestions for improvement. Ann R Coll Surg Engl. 2015;97(6):460-465. doi: https://doi.org/10.1308/rcsann.2015.0027.
Weber WP, Marti WR, Zwahlen M, Misteli H, Rosenthal R, Reck S, et al. The timing of surgical antimicrobial prophylaxis. Ann Surg. 2008;247(6):918-926. doi: https://doi.org/10.1097/SLA.0b013e31816c3fec.
Steinberg JP, Braun BI, Hellinger WC, Kusek L, Bozikis MR, Bush AJ, et al. Trial to Reduce Antimicrobial Prophylaxis Errors (TRAPE) Study Group. Timing of antimicrobial prophylaxis and the risk of surgical site infections: results from the Trial to Reduce Antimicrobial Prophylaxis Errors. Ann Surg. 2009;250(1):10-16. doi: https://doi.org/10.1097/SLA.0b013e3181ad5fca
Hawn MT, Richman JS, Vick CC, Deierhoi RJ, Graham LA, Henderson WG, et al. Timing of surgical antibiotic prophylaxis and the risk of surgical site infection. JAMA Surg. 2013;148(7):649-657. doi: https://doi.org/10.1001/jamasurg.2013.134.
Roberts JA, Abdul-Aziz MH, Davis JS, Dulhunty JM, Cotta MO, Myburgh J, et al. Continuous versus intermittent β-lactam infusion in severe sepsis. A meta-analysis of individual patient data from randomized trials. Am J Respir Crit Care Med. 2016;194(6):681-691. doi: https://doi.org/10.1164/rccm.201601-0024OC.
Knox MC, Edye M. Adherence to surgical antibiotic prophylaxis guidelines in New South Wales, Australia: identifying deficiencies and regression analysis of contributing factors. Surgical Infect. 2016;17(2):203-209. doi: https://doi.org/10.1089/sur.2015.195.
Putnam LR, Chang CM, Rogers NB, Podolnick JM, Sakhuja S, Matusczcak M, et al. Adherence to surgical antibiotic prophylaxis remains a challenge despite multifaceted interventions. Surg. 2015;158(2):413-419. doi: https://doi.org/10.1016/j.surg.2015.04.013.
Van Kasteren ME, Kullberg BJ, De Boer AS, Mintjes-de Groot J, Gyssens IC. Adherence to local hospital guidelines for surgical antimicrobial prophylaxis: a multicentre audit in Dutch hospitals. J Antimicrob Chemother. 2003;51(6):1389-1396. doi: https://doi.org/10.1093/jac/dkg264.
Dellinger EP, Hausmann SM, Bratzler DW, Johnson RM, Daniel DM, Bunt KM, et al. Hospitals collaborate to decrease surgical site infections. Am J Surg. 2005;190(1):9-15. doi: https://doi.org/10.1016/j.amjsurg.2004.12.001.
Yalcin AN, Serin S, Gurses E, Zencir M. Surgical antibiotic prophylaxis in a Turkish university hospital. J Chemother. 2002;14(4):373-377.
Finkelstein R, Reinhertz G, Embom A. Surveillance of the use of antibiotic prophylaxis in surgery. Isr J Med Sci. 1996;32(11):1093-1097.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


