Bacteriological profile and its antibiotic susceptibility in patients with urinary tract infection in tertiary care hospital
Abstract
Introduction: Urinary tract infections (UTIs) are counted among the most common infections in humans. In spite of the availability and use of antimicrobial drugs, UTIs caused by bacteria have been showing increasing trends. The extensive and inappropriate use of antimicrobial agents has invariably resulted in the development of antibiotic resistance which, in recent years, has become a major problem worldwide.
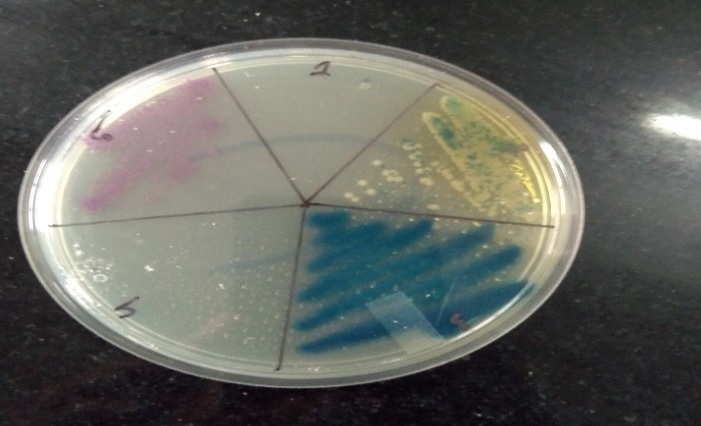
Materials and Methods: The study was conducted among the different ages of groups of both males and females attending KPC Medical College, Jadavpur, Kolkata during six months of the period included in this study. A total of 350 urine samples received from patients of the ICU and other wards of the medical college and hospital. All urine samples were processed within 1 hour after collection for aerobic bacterial culture.
Results: Out of a total of 380 patients, isolates were detected in 350 (76.29%) samples. Out of these, 280 (80%) were female. The most common organism found positive was Escherichia Coli. E. coli was highly sensitive to Amikacin and Nitrofurantoin. Whereas, E.coli was highly resistant to Ampicillin and Nalidixic acid. The antibiotic sensitivity pattern of Klebsiella and Acinetobacter shows that they were also highly sensitive to Amikacin. Klebsiella and Acinetobacter were highly resistant to Ampicillin and Gentamicin.
Conclusion: The pattern of resistance to commonly used antibiotics for treating UTI alerts us against indiscriminate usage of antibiotics.
Downloads
References
Shalini, Joshi MC, Rashid MK, Joshi HS. Study of Antibiotic Sensitivity Pattern in Urinary Tract Infection At A Tertiary Hospital. Nat J Integ Res Med. 2011;2(3):43-46.
Levi ME, Redington J, Barth L. The Patient with Urinary Tract Infection. Manual of Nephrology 6th Edition. Lippincott Williams & Wilkins. 2005;7:91.
Salek, SB., 1992. Infective syndrome in medical microbiology, 4th edition, pp. 740.
Goldstein FW. Antibiotic susceptibility of bacterial strains isolated from patients with community-acquired urinary tract infections in France. Multicentre Study Group. Eur J Clin Microbiol Infect Dis. 2000;19(2):112-117. doi: https://doi.org/10.1007/s100960050440.
Ashkenazi S, EvenTov S, Samra Z, Dinari G. Uropathogens of various childhood populations and their antibiotic susceptibility. Pediatr Infect Dis J. 1991;10(10):742-746. doi: https://doi.org/10.1097/00006454-199110000-00005.
Moore KN, Day RA, Albers M. Pathogenesis of urinary tract infections: a review. J Clin Nurs. 2002;11(5):568-574. doi: https://doi.org/10.1046/j.1365-2702.2002.00629.x.
Johnson JR. Virulence factors in Escherichia coli urinary tract infection. Clin Microbiol Rev. 1991;4(1):80-128. doi: https://doi.org/10.1128/CMR 4.1.80.
Kass, E. II.: Bacteriuria and diagnosis of infections of urinary tract. Arch. Intern. Med. 1957;100(5):709-714. doi: https://doi.org/10.1001/archinte.1957.00260110025004.
National Committee for Clinical Lab Standards, Performance Standardization for Antimicrobial Disc Susceptibility test. 4th ed. Villanona PA. CC 1993; DC M2 AS.
District laboratory Practice in Tropical Countries Monika Cheesbrough, 2nd Edition 2006.
Koneman’s Textbook of Diagnostic Microbiology,6th Edition 2005.
New FIC. Urinary tract infections. Am J Med. 1996; 100.
R Ananthanarayan, C K Jayaram paniker, Staphylococcus aureus. In Ananthanarayan & paniker’s Textbook of Microbiology. 8th ed: University press (India) pvt. Ltd; 2009.
Washington Winn Junior, Stephen Allen, William Janda et al. The Enterobacteriaecae. In Peter Darcy, Nancy Peterson, eds. Konemans colour atlas and textbook of diagnostic microbiology. 6th ed.: Lippincott, William and Wilkins; 2006;211-306.
Gold HS, Moellering RC, Berman JD, King M, Edwards N, Omar MT, Jackman AL, Boyle FT, Harrap KR, Borst P, Quellette M. Mackie and McCartney, Practical Medical Microbiology. J Biol Sci. 1996;4(4):1445-1453.
Tian SF, Chen BY, Chu YZ, Wang S. Prevalence of rectal carriage of Extended spectrum β-lactamase-producing Escherichia coli among elderly People in community settings in China. Can J Microbiol. 2008; 54(9):781-785. doi: https://doi.org/10.1139/w08-059.
Sanchez GV, Master RN, Karlowsky JA, Bordon JM. In vitro antimicrobial resistance of urinary Escherichia coli isolates among US outpatients from 2000 to 2010. Antimicrob Agents Chemother. 2012;56(4):2181-2183. doi: https://doi.org/10.1128/aac.06060-11.
Gupta K, Hooton T.M, Naber K.G, Wullt B, Colgan R, Miller L.G, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52(5):e103-20. doi: https://doi.org/10.1093/cid/ciq257.
Niranjan V, Malini A. Antimicrobial resistance pattern in Escherichia coli causing urinary tract infection among inpatients Indian J Med Res. 2014;139(6):945-948. Available from: http://www.ijmr.org.in/text.asp?2014/139/6/945/138080.
Gupta K, Stamm WE. Pathogenesis and management of recurrent urinary tract infections in women. World J Urol. 1990;17(6):415-420. doi: https://doi.org/10.1007/s003450050168.
Scottish Intercollegiate Guidelines Network. Management of suspected bacterial urinary tract infection in adults: a national clinical guideline. 2015. Available at http://www.sign.ac.uk/guidelines/fulltext/88/.
Hertz FB, Nielsen JB, Schønning K, Littauer P, Knudsen JD, Løbner-Olesen A, et al. Population structure of drug-susceptible, −resistant and ESBL producing Escherichia coli from community-acquired urinary tract infections. BMC Microbiol. 2016;16:1-6. doi: https://doi.org/10.1186/s12866-016-0681-z.
Akoachere JF, Yvonne S, Akum NH, Seraphine EN, Etilogic profile and anti-microbial susceptibility of community acquired UTI in two Cameroonian towns. BMC Res Notes 2012;5:219. doi: https://doi.org/10.1186/1756-0500-5-219.
Ejay H, Zafa A, Mahmood S, Javed MM. UTI infections caused by ESBL producing E-coli, K. pneumoniae. Afr J Biotechnol. 2011;10(73):16661-16666. doi: https://doi.org/10.5897/AJB11.2449.
Hryniewicz K, Szczypa K, Sulikowska A, Jankowski K, Betlejewska K, Hryniewicz W. Antibiotic susceptibility of bacterial strains isolated from urinary tract infections in Poland. J Antimicrob Chemother. 2001;47(6):773-780. doi: https://doi.org/10.1093/jac/47.6.773.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


