Granulomatous lesions !! Expected guests in unexpected places
Abstract
Introduction: Granulomatous lesions in various sites have different modes of presentation, different etiologic factors with identical histological patterns. The aim was to study the occurrence of granulomatous lesions at uncommon sites.
Materials and methods: A retrospective study of histopathological specimens received over a period of one year from June 2017 to May 2018 was done and cases of granulomatous lesions of various sites reported on histopathological examination were reviewed along with Ziehl-Neelsen (ZN) and Fite-Faraco (FF) staining.
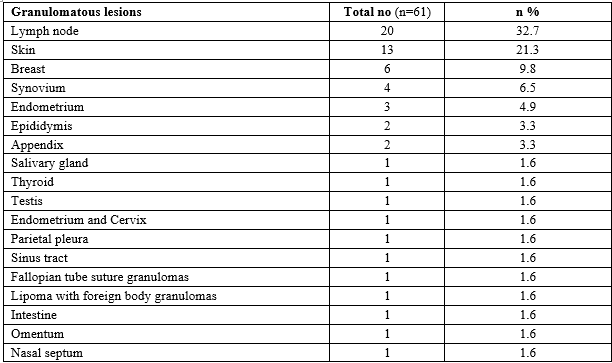
Results: Out of total 3623 histopathology specimens, 61 (1.7%) were granulomatous lesions of which 28 (45.9%) were AFB (Acid-fast bacilli) positive. 20 cases (32.7%) were granulomatous lymphadenitis out of which 12 (19.6%) were positive for AFB. 4 (6.5%) out of 13 (21.3%) granulomatous skin lesions showed AFB positivity. 6 (9.8%) cases of granulomatous mastitis (1 was AFB +ve), 4(6.5%) cases of granulomatous synovitis (2 were AFB +ve), 3 (4.9%) cases of granulomatous endometritis (2 were AFB+ve) were seen. 2 (3.3%) cases each of granulomatous epididymitis and appendicitis were noted. 1(1.6%) case of HIV positive hysterectomy specimen showed positivity for AFB. 1 (1.6%) case each of granulomatous lesions was found in the salivary gland, thyroid, testis, parietal pleura, nasal septum, suture granuloma of the fallopian tube, lipoma with foreign body granuloma, sinus tract, intestine, and omentum.
Conclusion: In the present study tuberculosis was the most common cause of granulomatous lesions of various sites. Histopathology plays an important role in the diagnosis and management of a variety of granulomatous lesions. Special stains play a vital role in the diagnosis of infectious granulomatous lesions.
Downloads
References
Kumar V, Abbas AK, Aster JC. Robbins and Cortran pathologic basis of disease. 9th ed; New Delhi, Elsevier; 2016:p 97-99.
James DG. A clinicopathological classification of granulomatous disorders. Postgrad Med J. 2000;76(898):457-465. doi: https://dx.doi.org/10.1136%2Fpmj.76.898.457.
Zumla A, James DG. Granulomatous infections: etiology and classification. Clin Infect Dis. 1996;23(1):146-156. doi: https://doi.org/10.1093/clinids/23.1.146.
James DG. What makes granulomas tick? Thorax. 1991;46:734-736.
James DG. Granuloma formation signifies a Th1 cell profile. Sarcoidosis. 1995;12(2):95-97.
Roman J, Jeon YJ, Gal A, Perez RL. Distribution of extracellular matrices, matrix receptors, sand transforming growth factor-1 in human and experimental living granulomatous inflammation. Am J Med Sci 1995;309(3):124-133. doi: https://doi.org/10.1097/00000441-199503000-00002.
Shah KK, Pritt BS, Alexander MP. Histopathologic review of granulomatous inflammation. J Clin Tuberc Other Mycobact Dis. 2017;7:1-12. doi: https://doi.org/10.1016/j.jctube.2017.02.001.
Guler M, Simsek A, Ofluglu R, Erguden HC, Capan N. Are all granulomatous lesions tuberculosis? Resp Med Case Reports. 2012;5:42-44. doi: https://dx.doi.org/10.1016%2Fj.rmedc.2011.10.001.
Debi U, Ravisankar V, Prasad KK, Sinha SK, Sharma AK. Abdominal tuberculosis of the gastrointestinal tract: Revisited. World J Gastroenterol. 2014;20(40):14831-14840.
Gautam K, Pai RR, Bhat S. Granulomatous lesions of the skin. J Pathol Nepal. 2011;1(2):81-86. doi: https://doi.org/10.3126/jpn.v1i2.5397.
Gandhare A, Mahashur A. Tuberculosis of the lymph nodes: many facets, many hues. Astrocyte. 2017;4(2):80-86. Available from: http://www.astrocyte.in/text.asp?2017/4/2/80/219475.
Sousa RD, Patil R. Breast tuberculosis or granulomatous mastitis: A diagnostic dilemma. Ann Trop Med PH. 2011;4(2):122-125. Available from: http://www.atmph.org/text.asp?2011/4/2/122/85767.
Vijay PM, Doddikoppad MM. Clinicopathological study of inflammatory synovial lesions. Int J Biol Med Res. 2011;2(4):882-888.
Mah EL, Bux S. Tuberculous synovitis of the knee with unusually thick synovial granulation tissue: A Case Report. Internet J Ortho Surg. 2006;6(2):1-5. Available at http://ispub.com/IJOS/6/2/12162.
Dincel O, Goksu M, Turk BA, Pehlivanoglu B, Isler S. Incidental findings in routine histopathological examination of appendectomy specimens; retrospective analysis of 1970 patients. Indian J Surg. 2016;88(6):1-7. doi: https://doi.org/10.1007/s12262-016-1557-z.
Cek M, Sturdza L, Pilatz A. Acute and chronic epididymitis. Europe Urol Suppl. 2017;16(4):124-131. doi: https://dx.doi.org/10.1016/j.eursup.2017.01.003.
Duggal S, Duggal N, Hans C, Mahajan RK. Female genital tuberculosis and HIV co-infection: case report 2009;27(4):361-363. Available from: http://www.ijmm.org/text.asp?2009/27/4/361/55461.
Gadgil NM, Ranadive NU, Sachdeva M. Granulomatous orchitis - a case report. Indian J Urol. 2001;18(1):92-94. Available from: http://www.indianjurol.com/text.asp?2001/18/1/92/37470.
Brunson J, Press HC, Hong IS. Granulomatous orchitis. J Nat Med Assoc. 2000;92(9):458-459.
Meachim G, Young MH. De Quervain's subacute granulomatous thyroiditis: histological identification and incidence. J Clin Path. 1963;16(3):189-199. doi: https://dx.doi.org/10.1136%2Fjcp.16.3.189.
Williams G, Sindwani R, Chandra R. Granulomatous diseases of sinonasal tract. Rhinology and Facial Plastic Surgery. 2009:321-333. doi: https://doi.org/10.1007/978-3-540-74380-4_28.
Valencia MP, Castillo M. Congenital and acquired lesions of the nasal septum: A practical guide for differential diagnosis. Radiographics. 2008;28(1):205-223. doi: https://doi.org/10.1148/rg.281075049.
Goldblum JR, Lamps LW, Mckenney JK, Myers JL. Rosai and Ackerman’s surgical pathology. 11th ed, Philadelphia, Elsevier,2018;p 236-237.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


