Association of biofilm production in ESBL and MBL producing clinical isolates of Pseudomonas aeruginosa
Abstract
Introduction: Pseudomonas aeruginosa is one of the most prevalent nosocomial pathogens that cause a life-threatening infection. One of the important characteristics of P. aeruginosa is biofilm formation and the most studied bacterium related to biofilm formation so far. The biofilm formation and beta-lactamases production synergistically contribute to the extensive dissemination of multi-drug resistant strains.
Aim: The present study was conducted to identify, biofilm-producing isolates of P. aeruginosa along with their antibiotic resistance pattern and ESBL and MBL production and to analyze their antibiogram.
Materials and methods: Various clinical specimens were collected and totally 82 clinical isolates of P. aeruginosa were included in this study. Biofilm producing isolates were identified by the tube adherence method.
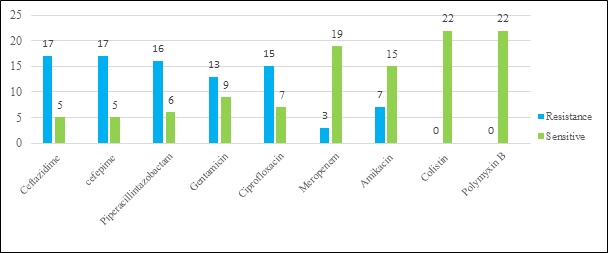
Results: Among the total, 22 [26.83%] isolates were biofilm producers and the maximum number was obtained from blood [100%], followed by ETT [75%], and Drain [66.67%]. Biofilm producing isolates were showing more resistance in comparison to non-biofilm producers. All isolates of P. aeruginosa were sensitive to colistin and polymyxin B. Association of ESBL production and biofilm formation found to be statistically significant [p < 0.002], which was a contrast to association of MBL production and biofilm formation.
Conclusion: High-level resistance to antimicrobial agents is a characteristic feature of infection caused by biofilm and lead to chronic infections. Knowledge about these biofilm-producing isolates is important in the clinical setting to eradicate these chronic and life-threating infections.
Downloads
References
Haji SH. Detection of Biofilm Formation in Pseudomonas aeruginosa Isolates from Clinical Specimens. Zanco J Pure Appl Sci. 2018; 30[4]:83-89. doi: https://doi.org/10.21271/ZJPAS.30.4.9
Saha S, Devi KM, Damrolien S, Devi KS, . K, Sharma KT. Biofilm production and its correlation with antibiotic resistance pattern among clinical isolates of Pseudomonas aeruginosa in a tertiary care hospital in north-east India. Int J Adv Med. 2018;5[4]:964. doi: http://dx.doi.org/10.18203/2349-3933.ijam20183129
Vallés J, Mariscal D, Cortés P, Coll P, Villagrá A, Díaz E, et al. Patterns of colonization by Pseudomonas aeruginosa in intubated patients: A 3-year prospective study of 1,607 isolates using pulsed-field gel electrophoresis with implications for prevention of ventilator-associated pneumonia. Intensive Care Med. 2004; 30[9]:1768-1775. doi: https://doi.org/10.1007/s00134-004-2382-6.
Gales AC, Jones RN, Turnidge J, Rennie R, Ramphal R. Characterization of Pseudomonas aeruginosa Isolates: Occurrence Rates, Antimicrobial Susceptibility Patterns, and Molecular Typing in the Global SENTRY Antimicrobial Surveillance Program, 1997–1999. Clin Infect Dis. 2001; 32[s2]:S146–S155. doi: https://doi.org/10.1086/320186.
Costerton JW. Cystic fibrosis pathogenesis and the role of biofilms in persistent infection. Vol. 9, Trends in Microbiology. 2001. p. 50-52. doi: https://doi.org/10.1016/s0966-842x(00)01918-1 [PMID:11173226]
Sharma D, Misba L, Khan AU. Antibiotics versus biofilm: An emerging battleground in microbial communities. Antimicrob Resist Infect Control. 2019;8[1]:1–10. doi: https://doi.org/10.1186/s13756-019-0533-3.
Gebreyohannes G, Nyerere A, Bii C, Sbhatu DB. Challenges of intervention, treatment, and antibiotic resistance of biofilm-forming microorganisms. Heliyon. 2019;5[8]:e02192. doi: https://doi.org/10.1016/j.heliyon.2019.e02192.
Høiby N, Ciofu O, Johansen HK, Song ZJ, Moser C, Jensen PØ, et al. The clinical impact of bacterial biofilms. Int J Oral Sci. 2011;3[2]:55–65. doi: https://doi.org/10.4248/IJOS11026.
Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: A common cause of persistent infections. Vol. 284, Science. 1999. p. 1318–1322. doi: https://doi.org/10.1126/science.284.5418.1318.
Ali, Syed Sajeed and Wakte PS. Isolation and identification of biofilm forming pseudomonas aeruginosa pseudomonas aeruginosa from wounds infection. Int J Curr Res. 2016;8[09]:38974–7.
Bose S, Khodke M. Detection Of Biofilm Producing Staphylococci: Need Of The Hour. J Clin Diagnostic Res. 2009;[3]:1915-1920.
Dumaru R, Baral R, Shrestha LB. Study of biofilm formation and antibiotic resistance pattern of gram-negative Bacilli among the clinical isolates at BPKIHS, Dharan. BMC Res Notes. 2019;12[1]:1–6. doi: https://doi.org/10.1186/s13104-019-4084-8.
Patricia M.Tille. Traditional cultivation and identification. In: Baily and Scott’s Diagnostic microbiology. 14th ed. Canada: Elsevier; 2017. p. 86–112.
Wayne P. CLSI,Performance Standards for Antimicrobial Susceptibility Testing. In: CLSI Supplement M100. 28th ed. 2018.
Yong D, Lee K, Yum JH, Shin HB, Rossolini GM, Chong Y. Imipenem-EDTA disk method for differentiation of metallo-beta-lactamase-producing clinical isolates of Pseudomonas spp. and Acinetobacter spp. J Clin Microbiol. 2002 Oct;40[10]:3798–801. doi: https://doi.org/10.1128/jcm.40.10.3798-3801.2002.
Christensen GD, Simpson WA, Younger JJ, Baddour LM, Barrett FF, Melton DM, et al. Adherence of coagulase-negative staphylococci to plastic tissue culture plates: A quantitative model for the adherence of staphylococci to medical devices. J Clin Microbiol. 1985;22[6]:996–1006.PMID: 3905855
Obritsch MD, Fish DN, MacLaren R, Jung R. Nosocomial infections due to multidrug-resistant Pseudomonas aeruginosa: Epidemiology and treatment options. Vol. 25, Pharmacotherapy. 2005. p. 1353–64. doi: https://doi.org/10.1592/phco.2005.25.10.1353.
Aloush V, Navon-Venezia S, Seigman-Igra Y, Cabili S, Carmeli Y. Multidrug-resistant Pseudomonas aeruginosa: Risk factors and clinical impact. Antimicrob Agents Chemother. 2006 Jan;50[1]:43–8. doi: https://doi.org/10.1128/AAC.50.1.43-48.2006.
Heydari S and Eftekhar F. Biofilm Formation and β-Lactamase Production in Burn Isolates of Pseudomonas aeruginosa. Jundishapur J Microbiol . 2015;8[[3]]:e15514. doi: https://doi.org/10.5812/jjm.15514.
Baniya B, Pant ND, Neupane S, Khatiwada S, Yadav UN, Bhandari N, et al. Biofilm and metallo beta-lactamase production among the strains of Pseudomonas aeruginosa and Acinetobacter spp. at a tertiary care hospital in Kathmandu, Nepal. Ann Clin Microbiol Antimicrob. 2017;16[1]:6–9. doi: https://doi.org/10.1186/s12941-017-0245-6.
Shrestha R, Nayak N, Bhatta DR, Hamal D, Subramanya SH, Gokhale S. Drug Resistance and Biofilm Production among Pseudomonas aeruginosa Clinical Isolates in a Tertiary Care Hospital of Nepal. Nepal Med Coll J. 2019;21[2]:110-116. doi: https://doi.org/10.3126/nmcj.v21i2.25109
Gurung J, Khyriem AB, Banik A, Lyngdoh WV, Choudhury B, Bhattacharyya P. Association of biofi lm production with multidrug resistance among clinical isolates of Acinetobacter baumannii and Pseudomonas aeruginosa from intensive care unit. Indian J Crit Care Med. 2013;17[4]:214-218. doi: https://doi.org/10.4103/0972-5229.118416.
Rewatkar AR. Staphylococcus aureus and Pseudomonas aeruginosa- Biofilm formation Methods. IOSR J Pharm Biol Sci. 2013;8[5]:36–40.
Revdiwala S, Rajdev BM, Mulla S. Characterization of bacterial etiologic agents of biofilm formation in medical devices in critical care setup. Crit Care Res Pract. 2012;2012:1–6. doi: https://doi.org/10.1155/2012/945805.
Basak S, N. M, O. R, Kumar Mallick S. Biofilms: A Challenge to Medical Fraternity in Infection Control. In: Infection Control. Available at- https ://doi.org/; 2013.
Nepal et al. Is there correlation of biofilm formation with multidrug resistance and ESBL production in pseudomonas aeruginosa ? Eur J Biomed Pharm Sci. 2017;4[01]:366–72. Available at-http://www.ejbps.com
Angel Díaz M, Ramón Hernández J, Martínez-Martínez L, Rodríguez-Baño J, Pascual A. Extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in Spanish hospitals: 2nd multicenter study [GEIH-BLEE project, 2006]. Enferm Infecc Microbiol Clin. 2003;21[2]:503-510. doi: https://doi.org/10.1016/j.eimc.2008.09.006.
Singh S, Singh SK, Chowdhury I, Singh R. Understanding the Mechanism of Bacterial Biofilms Resistance to Antimicrobial Agents. Open Microbiol J. 2017;11[1]:53–62. doi: https://doi.org/10.2174/1874285801711010053.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


