Testicular regression syndrome: A series of 22 cases at a tertiary care hospital
Abstract
Testicular regression syndrome (TRS) represents a congenital condition in which no normal testicular tissue can be identified following exploration for a clinically impalpable testis. It is seen in less than 5% of cryptorchidism cases, however accounts for 35-60% of clinically impalpable testis. To study the Clinicopathological spectrum of Testicular regression syndrome (TRS) and review the literature.
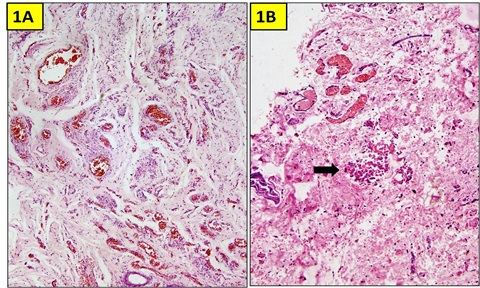
Study design: The study included 22 patients with nonpalpable testis, who had undergone resection of testicular nubbins. Original diagnosis was studied in context of pathological recognition of TRS and additional sections and stains were examined. Pathological assessment included identification of epididymis and vas deferens, vascularised fibrous nodule (VFN), dystrophic calcification, hemosiderin and pampiniform plexus like veins. Stain for iron and calcium were performed. On secondary review, 21 out of 26 cases of undescended testis (UDT) showed features consistent with the diagnosis of TRS. On microscopy, VFN was observed in 17 (77.3%), calcification in 4 (18.2%), hemosiderin in 15 (68.2%), vas deferens in 13 (59%), epididymis in 11 (50%), prominent vessels in 21 (95.4%) and seminiferous tubules in 6 (27.3%) cases. The presence of dystrophic calcification and hemosiderin deposition with absent viable tissue points to the hypoxic injury to the testis. TRS theoretically carries a long-term risk for malignant degeneration therefore In the typical situation in which a blind-ending spermatic cord without viable testis is submitted for tissue analysis, it is imperative to characterize such cases as consistent with regressed testis thus eliminating the need for further surgical intervention.
Downloads
References
Spires SE, Woolums CS, Pulito AR, Spires SM. Testicular regression syndrome: a clinical and pathologic study of 11 cases. Arch Pathol Lab Med. 2000;124(5):694-698. doi: https://doi.org/10.1043/0003-9985(2000)124%3C0694:trs%3E2.0.co;2.
Pirgon Ö, Dündar BN. Vanishing testes: a literature review. J Clin Res Pediatr Endocrinol. 2012;4(3):116-120. doi: https://doi.org/10.4274/jcrpe.728.
Hegarty PK, Mushtaq I, Sebire NJ. Natural history of testicular regression syndrome and consequences for clinical management. J Pediatr Urol. 2007;3(3):206-208. doi: https://doi.org/10.1016/j.jpurol.2006.08.007.
Selby DM. Sexual maldevelopment syndromes. In: Stocker JT, Dehner LP, eds. Pediatric Pathology Philadelphia, Pa: JB Lippincott Co. 1992:117-159.
Redman F. Impalpable testis: observations based on 208 consecutive operations for undescended testis. J Urol. 1980;124(3):379-381. doi: https://doi.org/10.1016/s0022-5347(17)55457-9.
Smolko MJ, Kaplan GW, Brock WA. Location and fate of the nonpalpable testis in children. J Urol. 1983;129(6):1204-1206. doi: https://doi.org/10.1016/s0022-5347(17)52643-9.
Desai A, Verma R, Parab M. A Case of Testicular Regression Syndrome. Int J Surg. 2008;21:2.
Ferro F, Lais A, Bagolan P, Talamo M, Caterino S. Impact of primary surgical approach in the management of impalpable testis. Eur Urol. 1992;22(2):142-146. doi: https://doi.org/10.1159/000474742.
Bader MI, Peeraully R, Ba'ath M, McPartland J, Baillie C. The testicular regression syndrome--do remnants require routine excision? J Pediatr Surg. 2011;46(2):384-386. doi: https://doi.org/10.1016/j.jpedsurg.2010.11.018.
Smith NN, Byard RW, Bourne AJ. Testicular regression syndrome: a pathological study of 77 cases. Histopathol. 1991;19(3):269–272. doi: https://doi.org/10.1111/j.1365-2559.1991.tb00033.x.
Mizuno K, Kojima Y, Kamisawa H, Kurokawa S, Moritoki Y, Nishio H, et al. Feasible etiology of vanishing testis regarding disturbance of testicular development: histopathological andimmunohistochemical evaluation of testicular nubbins. Int J Urol. 2012;19(5):450-456. doi: https://doi.org/10.1111/j.1442-2042.2011.02951.x.
Wright JE. The ‘‘atrophic’’ testicular remnant: atrophy or agenesis? Pediatr Surg Int. 1986;1:229-231. doi: https://doi.org/10.1007/BF00177152.
Schned AR, Cendron M. Pathologic findings in the vanishing testes syndrome. J Urol Pathol. 1997;6:95-107.
Sutcliffe JR, Wilson-Storey D, Smith NM. Ante-natal testicular torsion: only one cause of the testicular regression syndrome? J R Coll Surg Edinb. 1996;41(2):99-101.
Honore LH. Unilateral anorchism. Report of 11 cases with discussion of etiology and pathogenesis. Urol. 1978;11(3):251-254. doi: https://doi.org/10.1016/0090-4295(78)90126-7.
Law H, Mushtaq I, Wingrove K, Malone M, Sebire NJ. Histopathological features of testicular regression syndrome: relation to patient age and implications for management. Fetal Pediatr Pathol. 2006;25(2):119-129. doi: https://doi.org/10.1080/15513810600788806.
Van Savage JG. Avoidance of inguinal incision in laparoscopically confirmed vanishing testis syndrome. J Urol. 2001;166(4):1421-1424. doi: https://doi.org/10.1097/00005392-200110000-00060.
Storm D, Redden T, Aguiar M, Wilkerson M, Jordan G, Sumfest J. Histologic evaluation of the testicular remnant associated with the vanishing testes syndrome: is surgical management necessary? Urol. 2007; 70(6):1204-1206. doi: https://doi.org/10.1016/j.urology.2007.08.020.
Merry C, Sweeney B, Puri P. The vanishing testis: anatomical and histological findings. Eur Urol. 1997; 31(1):65-67. doi: https://doi.org/10.1159/000474420.
Belman AB, Rusthon HG. Is the vanished testis always a scrotal event? Br J Urol Int. 2001;87(6):480-483. doi: https://doi.org/10.1046/j.1464-410x.2001.00101.x.
Rozanski TA, Wojno KJ, Bloom DA. The remnant orchiectomy. J Urol. 1996;155(2):712-714.
Cendron M, Schned AR, Ellsworth PI. Histological evaluation of the testicular nubbin in the vanishing testis syndrome. J Urol. 1998;160(3 Pt 2):1161-1162. doi: https://doi.org/10.1097/00005392-199809020-00054.
Marcantonio SM, Fechner PY, Migeon CJ, Perlman EJ, Berkovitz GD. Embryonic testicular regression sequence: a part of the clinical spectrum of 46, XY gonadal dysgenesis. Am J Med Genet. 1994;49(1):1-5. doi: https://doi.org/10.1002/ajmg.1320490102.
Williams EV, Appanna T, Foster ME. Management of the impalpable testis: a six year review together with a national experience. Postgrad Med J. 2001;77:320-322.
Emir H, Ayik B, Eliçevik M, Buyukunal C, Danişmend N, Dervişoglu S et al. Histological evaluation ofthe testicular nubbins in patients with nonpalpable testis: assessment of etiology andsurgical approach. Pediatr Surg Int. 2007;23(1):41-44. doi: https://doi.org/10.1007/s00383-006-1802-9.
Nishizawa S, Suzuki K, Tachikawa N, Nukui A, Kumamaru T, Shioji Y, et al. The vanishing testis: diagnosis and histological findings. Nippon Hinyokika Gakkai Zasshi. 2000;91(6):537-541. doi: https://doi.org/10.5980/jpnjurol1989.91.537.
Grady RW, Mitchell ME, Carr MC. Laparoscopic and histologic evaluation of the inguinal vanishing testis. Urol. 1998;52(5):866-869. doi: https://doi.org/10.1016/s0090-4295(98)00326-4.
Turek PJ, Ewalt DH, Snyder HM, Stampfers D, Blyth B, Huff DS et al. The absent cryptorchid testis: The absent cryptorchid testis: surgical findings and their implications for diagnosis and etiology. J Urol. 1994;151(3):718-720. doi: https://doi.org/10.1016/s0022-5347(17)35069-3.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


