Reactive thrombocytosis- etiology and its relationship with different hematological parameters, ESR, & CRP in Tuberculosis
Abstract
Background: The measurements of platelet count, mean platelet volume (MPV), WBC are routinely available nowadays. The aim of this study was to determine age dependent aetiology and relationship of these parameters whether they were associated with the known markers of disease activity, erythrocyte sedimentation rate (ESR) and C- reactive protein (CRP) in Tuberculosis.
Methods: This descriptive study was done on 500 patients with platelet count > 450,000/ μl and the cause being reactive. Platelet count, WBC, MPV, ESR, and CRP were measured at the time of hospitalization.
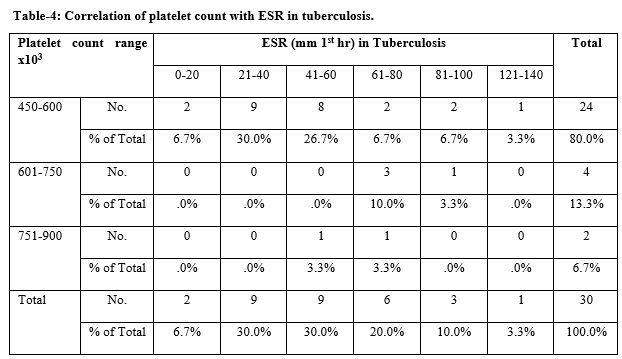
Result: Most common cause of reactive thrombocytosis was found to be infection (28.8%), tissue damage (16.4%), iron deficiency anemia (16.2%), malignancy (9.6%), inflammation (non-tuberculosis) (9.4%), diabetes mellitus (6.4%), tuberculosis (6.0%) respectively. There was low degree of positive correlation between reactive thrombocytosis with WBC (r = 0.337, P= 0.06) and ESR (r = .277, P= >0.05). There was low degree of negative correlation between reactive thrombocytosis and CRP (r= -.131, P= >0.05). There was significant negative correlation between reactive thrombocytosis and MPV (r = -.561, P= >0.001).
Conclusion: This study demonstrated a higher level of platelet count and lower MPV in all the patients having reactive thrombocytosis. The changes in these parameters (platelets count, WBC, MPV, CRP and ESR) may reflect a reaction to the inflammatory condition. Therefore, in endemic areas, the presence of such haematological peripheral blood changes may raise the suspicion of tuberculosis.
Downloads
References
Sanchez S, Ewton A. Essential Thrombocythemia. A review of diagnostic and pathologic features. Arch Pathol Lab Med. 2006;130(8):1144-1150. doi: https://doi.org/10.1043/1543-2165(2006)130[1144:ET]2.0.CO;2.
Vannucchi AM, Barbui T. Thrombocytosis and Thrombosis. Hematology American Society Hematology Education Program.2007;1:363-370. doi: https://doi.org/10.1182/asheducation-2007.1.363.
Schafer AI. Thrombocytosis. N Engl J Med. 2004;350(12):1211-1219. doi: https://doi.org/10.1056/NEJMra035363.
World Health Organization: WHO Expert committee on tuberculosis ninth report. WHO tech Research Series. 1974;552:1-40. Available at https://apps.who.int/iris/handle/10665/41095
Singh KJ, Ahluwalia G, Sharma SK, Saxena R, Chaudhary VP, Anant M. Significance of hematological associations in tuberculosis; JAPI. 2001;49(4):788-790.
Bozoky G, Ruby E, Góhér I, Tóth J, Mohos A. Hematologic abnormalities in pulmonary tuberculosis. Orv Hetil. 1997;138(17):1053-1056.
Yadav D, Chandra J, Sharma S, Singh V, Clinico-hematological Study of Thrombocytosis Indian J Pediatr 2010; 77(6):643-647. doi: https://doi.org/10.1007/s12098-010-0091-4.
Santhosh‐Kumar CR, Yohannan MD, Higgy KE, Al‐Mashhadani SA. Thrombocytosis in adults: analysis of 777 patients. J Intern Med. 1991;229(6):493-495. doi: https://doi.org/10.1111/j.1365-2796.1991.tb00383.x.
Buss DH, Cashell AW, O’Connor ML, Richards F, Douglas Case LD. Occurence, etiology, and clinical significance of extreme thrombocytosis: a study of 280 cases. Am J Med. 1994;96(3):247-253. doi: https://doi.org/10.1016/0002-9343(94)90150-3.
Sutor AH. Thrombocytosis in childhood. Sem Thromb Hemost. 1995;21(3):330-339. doi: https://doi.org/10.1055/s-2007-1000654.
Wolach B, Morag H, Drucker M, Sadan N. Thrombocytosis after pneumonia with empyema and other bacterial infections in children. Pediatr Infect Dis J. 1990;9(10):718-721. doi: https://doi.org/10.1097/00006454-199010000-00007.
Baynes RD, Bothwell TH, Flax H, McDonald TP, Atkinson P, Chetty N, et al, Reactive thrombocytosis in pulmonary tuberculosis. J Clin Pathol. 1987;40(6):676-679. doi: https://dx.doi.org/10.1136%2Fjcp.40.6.676.
Nagai T, Komatsu N, Sakata Y, Miura Y, Ozawa K. Iron deficiency anemia with marked thrombocytosis complicated by central retinal vein occlusion. Intern Med 2005;44(10):1090-1092. doi: https://doi.org/10.2169/internalmedicine.44.1090.
MC Donald TP. A comparison of platelet size, Platelet count 35s incorporation as assay for thrombopoietin. Br J Hematol. 1976;34(2):257-267. doi: https://doi.org/10.1111/j.1365-2141.1976.tb00196.x.
Omar M, Jogessar VR, Kamder MC. Thrombocytosis associated with tuberculosis peritonitis tubercle 1983;64(4):295-296. doi: https://doi.org/10.1016/0041-3879(83)90027-2.
Jain A. Tuberculosis of the spine a fresh look at an old disease. JBJS (Br) 2010;92(7):905-913. doi: https://doi.org/10.1302/0301-620X.92B7.24668.
Wilson D, Badri M, Maartens G. Performance of serum C-reactive protein as a screening test for smear negative tuberculosis in an ambulatory high HIV prevalence population. PLoS ONE. 2011;6(1):5248. doi: https://doi.org/10.1371/annotation/53a56437-a810-4373-baee-16685ec20b2f.
Muzaffar TM, Shaifuzain AR, Imran Y, Haslina MN. Haematological changes in tuberculosis spondylitis patients at the hospital university. Southeast Asian J Trop Med Publ Health. 2008;39(4):1997-2000.
Singh KJ, Ahulwalia G. Sharma SK, Saxena R, Chaudhary VP, Anant M. Significance of hematological manifestations in patients with tuberculosis, J Asso Physicians Ind. 2001;49:788-794.
Olaniyi JA, Aken, Ova YA. Bone marrow findings in patients with pulmonary tuberculosis. Afr J Med Sci. 2003;32(2):155-157.
Schlossberg D. Tuberculosis and nontuberculous mycobacterial infections. 4th Ed. Philadelphia, Pennsyvania, United States of America: W.B. Saunders Company;1999.
Banerjee M, Chaudhary BL, Shukla S, Hematological profile among pulmonary tuberculosis patients in tertiary care hospital. Int J Bioassays. 2015;4(5):3900-3902.
Yaranal PJ, Umashankar T, Harish SG. Hematological Profile in Pulmonary Tuberculosis. Int J Health Rehabil Sci. 2013;2(1):50-55.
Dunn R. The medical management of spinal tuberculosis. SA Orthop J. 2010;9(1):37-41.
Ukpe IS, Sothern L. Erythrocyte sedimentation rate values in active tuberculosis with and without HIV co-infection. SAMJ. 2006;96(5):427-428.
Guo LX, Ma YZ, Li HW, Xue HB, Peng W, Luo XB. Variety of ESR and C-reactive protein levels during peri-operative period in spinal tuberculosis (article in Chinese) Pub Med Zhonggno Gu Shang. 2010;3(23):200-202.
Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des. 2011;17(1):47-58. doi: https://doi.org/10.2174/138161211795049804.
Tozkoparan E, Deniz O, Ucar E, Bilgic H, Ekiz K, Changes in platelet count and indices in pulmonary tuberculosis. Clinic Chem Lab Med. 2007;45(8);1009-1013. doi: https://doi.org/10.1515/CCLM.2007.194.
F. Şahin, E. Yazar, and P. Yıldız. Prominent features of platelet count, plateletcrit, mean platelet volume and platelet distribution width in pulmonary tuberculosis. Multidisciplin Resp Med, 2012;7(38). doi: https://doi.org/10.1186/2049-6958-7-38.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


