The microbial burden in chronic suppurative otitis media patients along with their antibiogram
Abstract
Introduction: Chronic suppurative otitis media (CSOM) is a common health problem in countries with low socio-economic strata because of poor nutrition, population burden, low hygienic condition, insufficient health care, and repeated upper respiratory tract infection (URTI). Untreated cases of CSOM result in complications ranging from persistent otorrhoea, mastoiditis, labyrinthitis, facial nerve palsy to intracranial abscesses or thromboses. Microbiological profile and their antibiotic sensitivity pattern are essential to enable proper treatment of this disease and preventing the development of complications.
Material and Methods: The current study was designed to identify the pathogenic agents causing CSOM and to understand their antimicrobial resistance pattern who attended ENT Department of this hospital between July 2017 to June 2019.
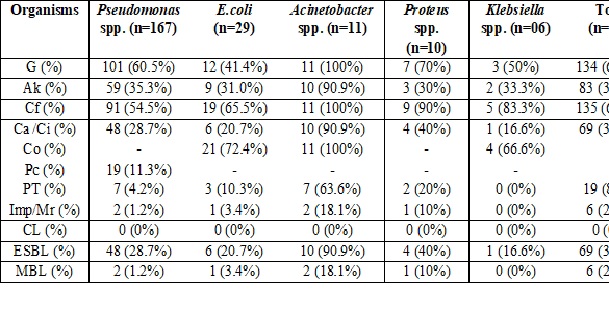
Results: Among 496 clinical samples, microbes were seen in 329 (66.3%) cases with predominant male (66.3%) distribution and age group of 11-20 years (31%). Pseudomonas spp. (50.7%) is predominantly isolated. It showed resistance to aminoglycosides and fluoroquinolones but was found sensitive to carbapenems with a resistance rate of 1.2%. ESBL (Extended-spectrum β- lactamase) detection was seen in 30.9% of GNB while MBL (Metallo β- lactamase) was detected in 2.7% of cases. S.aureus was highly resistant to first-line antibiotics with MRSA (Methicillin-resistant S.aureus) rate of 64.1%, however, all were sensitive to glycopeptides.
Conclusions: There should be a minimum gap between the onset of symptoms and the treatment provided to prevent complications of CSOM and also the complicated cases should be referred to specialized centers for better management.
Downloads
References
Chronic suppurative otitis media: Burden of Illness and Management Options. World Heath Organisation, 2004. Available at https://apps.who.int/iris/handle/10665/42941.
Prakash R, Juyal D, Negi V, Pal S, Adekhandi S, Sharma et al. Microbiology of chronic suppurative otitis media in a tertiary care setup in Uttarakhand state, India. North Am J Med Sci. 2013;5(4):282-287. doi: https://doi.org/10.4103/1947-2714.110436.
Bluestone CD, Klein JO. Microbiology. In: Bluestone CD, Klein JO, eds. Otitis Media in Infants and Children. 3rd ed. Philadelphia, PA: W. B. Saunders; 2001:79–1014.
Daly A. Knowledge and attitude about otitis media risk: implication for prevention. J Pediatr. 1997;100(6): 931-936. doi: https://doi.org/10.1542/peds.100.6.931.
Shrestha B L, Amatya R C M, Shrestha I, Ghosh I. Microbiological profile of chronic suppurative otitis media. Nepalese J ENT, Head and Neck Surg. 2011;2(2):6-7. doi: https://doi.org/10.3126/njenthns.v2i2.6793.
Clinical and Laboratory Standard Institute. Performance Standards for Antimicrobial Susceptibility Testing. Vol. 1, No. 1, M2 A9. Pennsylvania, USA: Clinical and Laboratory Standard Institute; 2013. Available at https://clsi.org/media/2663/m100ed29_sample.pdf.
Mansoor T, Musani MA, Khalid G, Kamal M. Pseudomonas aeruginosa in chronic suppurative otitis media: Sensitivity spectrum against various antibiotics in Karachi. J Ayub Med Coll Abbottabad. 2001;21(2):120-123.
Poorey VK, Lyer A. Study of bacterial flora in csom and its clinical significance. Indian J Otolaryngol Head Neck Surg. 2002;54(2):91-95. doi: https://doi.org/10.1007/bf02968724.
Kumar R, Srivastava P, Sharma M, Rishi S, Nirwan PS, Hemwani K et al. Isolation and antimicrobial sensitivity profile of bacterial agents in chronic suppurative otitis media patients at NIMS hospital, Jaipur. Int J Pharma Biol Sci.2013;3(4):265-269.
Malkappa KS, Kondapaneni S, Supam BR, Chakraverti KT. Study of bacterial isolates and their antibiotic susceptibility pattern in Chronic Supperative Otitis Media. Indian J Otol. 2012;18(3):136-139. doi: https://doi.org/10.4103/0971-7749.103440.
Parveen SS and Rao JR. Aerobic bacteriology of Chronic Suppurative Otitis Media (CSOM) in a teaching hospital. J Microbiol Biotechnol Res. 2012;2(4):586-589. doi: https://doi.org/10.9734/IJTDH/2015/13766.
Prayaga N, Moorthy S, Lingaiah J, Katari S, Nakirakanti A. Clinical Application of a Microbiological Study on Chronic Suppurative Otitis Media. Int J Otolaryngol Head Neck Surg. 2013;2(6):290-294. doi: http://dx.doi.org/10.4236/ijohns.2013.26060.
Aslam MA, Ahmed Z, Azim R. Microbiology and drug sensitivity patterns of chronic suppurative otitis media. J Coll Physicians Surg Pak. 2004;14(8):459-461.
Kumar H, Seth S. Bacterial and fungal study of 100 cases of chronic suppurative otitis media. J Clin Diagn Res. 2011;5:1224-1227.
Shyamla R, Reddy SP. The study of bacteriological agents of chronic suppurative otitis media–aerobic culture and evaluation. J Microbiol Biotechnol Res.2012;2:152-162.
Gulati SK. Investigative profile in patients of chronic suppurative otitis media. Indian J Otol. 1997;3(2):59-62.
Gaur RS, Mathew J, Varghese AM, Mathew GA, Chandrasekharan R, Anandan S. Microbiological pattern of ear swabs in chronically discharging ears in a Tertiary Care hospital in India. Indian J Otol. 2013;19(2):51-54. doi: https://doi.org/10.4103/0971-7749.113501.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


