Study of haematological parameters in malaria: a prospective study
Abstract
Background: A blood parasites plasmodia is responsible for malaria hence there are haematological alterations in malaria. The haematological changes that have been reported to accompany malaria include anaemia, thrombocytopenia, leucocytosis and leucopenia.
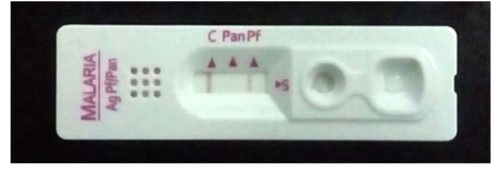
Methods: Total 585 smear positive malaria cases were taken and various haematological parameters were studied.
Results: Out of 585 smear positive cases, P. vivax was positive in 422 (72%) cases, while P. falciparum was positive in 160 (27%) cases and mixed infection was found in 3 (1%) cases. Anaemia was seen in 420 (71.79%) cases. Normocytic normochromic blood picture was the most common type in anaemic patients 223 (38.11%). Next common finding was Normocytic hypochromic RBCs 185 (31.62%). Microcytic hypochromic RBCs found in 152 (25.98%) cases. Thrombocytopenia was seen in total 490 (83.76%) of the patients. Moderate thrombocytopenia was more common and present in 409 (70%) of patients while Severe thrombocytopenia was seen in 81 (13.84%) of cases. In falciparum malaria thrombocytopenia was present in 90% of the patients while it was present in 81.27% of the patients in vivax malaria. 129 cases (22.05%) shows leucopoenia out of which 81 (13.84%) belong to P. vivax, 45 (7.69%) belong to P. falciparum and 3 (1%) were belong to mixed infection. Total Leucocyte Count was normal in 77.95 % of the patients.
Conclusions: Various haematological findings can help in early diagnosis of malaria which is essential for timely and appropriate treatment which can limit the morbidity and prevent further complications.
Downloads
References
Taylor TE, Strickland GT. Malaria. In: Strickland’s infectious Disease, 4th ed. London: Wiley. 2006:614-642.
Park K. Malaria. In Preventive and Social Medicine. 17th ed. Jabalpur Publishers Banarsidas Bhanot Publishers. 2002:192-201.
Surve KM, Kulkarni A.S, Rathod S.G, Bindu R.S. Study of haematological parameters in malaria. Int J Res Med Sci. 2017;5(6):2552-2557. doi: http://dx.doi.org/10.18203/2320-6012.ijrms20172446.
Rojanasthein S. Surakomolleart V, Boonpucknavig S, Isarangkura P. Hematological and coagulation studies in malaria. J Med Assoc Thai 1992;75(1):190-194.
Sharma SK, Das RK, Das BK, Das PK. Haematological and coagulation profile in acute falciparum malaria. J Assoc physicians India. 1992;40(9):581-583.
Horstmann Rd, Dietrich M, Bienzle U, Rasche. H malaria induced thrombocytopenia. Blut 1981;42(3):157-164.
Makkar Rps, Mukhopadhyay S, Monga A, Gupta A. Plasmodium vivax malaria presenting with severe thrombocytopenia. Braz J Infect Dis.2002;6(5):263-265.
Kakar A, Bhoi S, Prakash V, Kakar S. Profound thrombocytopenia in plasmodium vivax malaria. Diagn Microbiol Infect Dis. 1999;35(3):243-244. doi: https://doi.org/10.1016/s0732-8893(99)00069-3.
Sen R, Tewari Ad, Sehgal Pk, Singh U, Sikka R, Sen J. Clinico-haematological profile in acute and chronic plasmodium falciparum malaria in children. J Com Dis. 1994;26(1):31-38.
Warrell Da, Turner Gdh, Francis N. Pathology and pathophysiology of human malaria. In:gilles hm, warrell da, editors. Essential malariology 4th ed. London: Arnold. 2002;236-251.
Ladhani S, Lowe B, Cole Ao, Kowuondo K, Newton RJC. Changes in white blood cells and platelets in children with falciparum malaria: relationship to disease outcome. Brit J Haematol. 2002;119(3):839-847. doi: https://doi.org/10.1046/j.1365-2141.2002.03904.x.
WHO. Basic malaria microscopy. Part I. Learner’s guide. 2nd ed. Geneva: World Health Organization; 2010. p. 21.
90% of malarial deaths happen in rural India, Makarand Purohit, 2015, July 24. Available from http://www.impe-qn.org.vn/impe-qn/en/portal/InfoDetail.jsp?area58&cat=1025&ID=934.
Patel P, Vijapura T, Patel N, Gajjar D. Rising incidence of Malaria Ahmedabad; Gujarat, 2011- 2012. Int J Med Sci Public Health.2013;2(3):568-571. doi: http://dx.doi.org/10.5455/ijmsph.2013.160420131.
Kevadiya SM, Patel MM, Modi J, Gamit B, Patel PR, Padsada S. Characteristic and trends of malaria in Surat district of Gujarat: a hospital-based study. Int J Res Med Sci. 2014; 2(1):151-153. doi: https://dx.doi.org/10.5455/2320-6012.ijrms20140230.
Panchal PD, Trivedi MB, Shethwala N, Khatri HS. A study of prevalence and seasonal trends of different malarial species in district hospital. Int J Res Med Sci. 2016;4(9):4155-4157. doi: http://dx.doi.org/10.18203/2320-6012.ijrms20162952.
Solanki SJ, Shah R, Patel S, Singh N. Study of 100 cases of complicated plasmodium Falciparum malaria. Int J Sci Res. 2013;2(10):1-2.
Bashawri L., Mandil A., Bahnassy A., Ahmed M. Malaria: haematological aspects. Ann Saudi Med. 2002;22(5-6):372-377. doi: https://doi.org/10.5144/0256-4947.2002.372.
Richards MW, Behrens RH, Doherty JF. Hematologic changes in Acute, Imported Plasmodium falciparum Malaria. Am J Trop Med Hyg. 1998;59(6):859.
Echieverri M, Tobon A, Alvarez G, Carmona J, Blair S. Clinical and laboratory findings of plasmodium vivax malaria in colombia. Rev Inst Med Trop. 2003;45(1):29-34. doi: http://dx.doi.org/10.1590/S0036-46652003000100006.
Jadhav UM, Patkar VS, Kadam NN. Thrombocytopenia in Malaria - Correlation with Type and Severity of Malaria. J Assoc Physicians India. 2004;52(2):615-618.
Akhtar S., Raghvendra G., Mahore S., Maimoon S., Hematological changes in malaria:A comparative study. J Pharm Bio Sci. 2012;2(4):15-19. doi: https://dx.doi.org/10.9790/3008-0241519.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


