Isolation, Speciation and antifungal drug susceptibility of Candida species from clinically suspected infections in a tertiary care hospital
Abstract
Introduction: The incidence of fungal infections has increased dramatically over the last two to three decades. Study was done on, Clinical samples from suspected patients of candidiasis. Study period was one and a half year from January 2013 to June 2014. Out of 915 clinically suspected samples of candidiaisis processed in the Microbiology Laboratory, 156 (17.04%) yielded growth of Candida species.
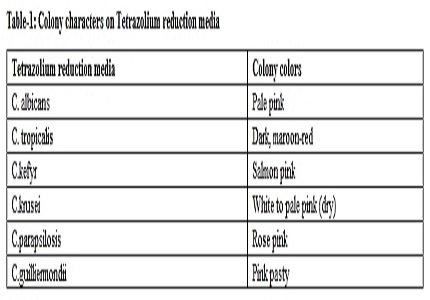
Methods: Candida was identified from Clinical samples by wet mount, Gram stain and Culture on SDA. The organisms were further speciated by germ tube test, Cornmeal agar Morphology, Sugar assimilation and Fermentation tests and CHROM agar. Antifungal susceptibility testing was done by disc diffusion method with Fluconazole (25 µg), Amphotericin-B(100U), Itraconazole(10 µg), Nystatin(50 µg), Clotrimazole(10 µg) and Voriconazole(1 µg).
Results: C.tropicalis (46.79%) was the most common species isolated followed by C.albicans (37.17%) and C.parapsilosis (9.61%). Non albicans Candida species(NAC) (62.82%) was more than C.albicans (37.17%). All species isolated were susceptible to Amphotericin-B(100U), Nystatin(50 µg) and Voriconazole(1µg). Resistance to commonly used antifungal agents was Fluconazole-20.40%, Clotrimazole-18.26% and Itraconazole-17.34%.
Conclusion: Species identification is important for treatment of Candida infections, as NAC species continue to be increasingly documented and not all species respond to same treatment.
Downloads
References
2. Patel, L., Pethani, J., Bhatia, P., Rathod, S., Shah, P. Prevalence of Candida Infection and its Antifungal Susceptibility Pattern in tertiary Care Hospital, Ahmedabad. Nat J Med Res. 2012; 2(4): 439-41.
3. Singh, T., Kashyap, A., Ahluwalia, G. et al. Epidemiology of fungal infections in critical care setting of a tertiary care teaching hospital in North India: a prospective surveillance study. J Clin Sci Res. 2014;3: 14-25.
4. Prasad KN, Agarwal J, Dixit AK et al. Role of yeasts as nosocomial pathogens & their susceptibility to fluconazole & amphotericin B. Indian J Med Res. 1999 Jul;110:11-7.
5. Paswan, A., Dinesh, C., Singh, D et al. Isolation and distribution of candida species among different clinical situations in critically ill patients: prospective study. International Journal of Biomedical Research. 2012; 3[2] :120‐126.
6. Chen XS, Yin YP, Liang GJ, Gong XD, Li HS, Shi MQ, Yu YH. Co-infection with genital gonorrhoea and genital chlamydia in female sex workers in Yunnan, China. Int J STD AIDS. 2006 May;17(5):329-32. [PubMed]
7. Topley and Wilson’s Microbiology and Microbial infections, Medical mycology. Chapter 30,Candidiasis, 579-620.
8. Deorukhkar SC, Saini S, Mathew S. Non-albicans Candida Infection: An Emerging Threat. Interdiscip Perspect Infect Dis. 2014;2014:615958. doi: 10.1155/2014/615958. Epub 2014 Oct 22. [PubMed]
9. Deorukhkar, S. C.; Saini, S. Species Distribution and Antifungal Susceptibility Profile of Candida Isolated from Various Clinical Specimens. Med Rev. 2014; 6(3) :11-15.
10. Chander J. Textbook of Medical Mycology, 3rd ed . Mehta publishers: 2012.
11. Fran Fisher and Norma B.Cook. Fundamentals of Diagnostic Mycology 1998; W.B. Saunders, Philadelphia. Pg 196-212.
12. Kashid, R., Sandhya, B., et al. Incidence of non-candida albicans in patients with urinary tract infection with special reference to speciation and antifungal susceptibility. J. of Evolution of Medical and Dental Sciences. 2012; 4(1): 577.
13. Deorukhkar, S., Saini, S. Laboratory approach for diagnosis of Candidiasis through ages. Int.J.Curr.Microbiol ,App.Sci . 2014; 3(1): 206-218.
14. Jha BJ, Dey S, Tamang MD, Joshy ME, Shivananda PG, Brahmadatan KN. Characterization of Candida species isolated from cases of lower respiratory tract infection. Kathmandu Univ Med J (KUMJ). 2006 Jul-Sep;4(3):290-4.
15. Amar, C., Hajare, V. et al. Prevalence and antifungal susceptibility of Candida Species Isolated from Patients Attending Tertiary Care Hospital. IOSR-JDMS. 2014; 13(5): 44 –49.
16. Clinical and laboratory Standards Institute (CLSI), August 2009. Method for antifungal disk diffusion susceptibility testing of Yeasts. Approved guideline-2nd ed. CLSI document-M44-A2, 29(17).
17. Wayne PA et al,2004 Method for Antifungal Disc Diffusion Susceptibility Testing of Yeasts, CLSI M-44A.
18. Jayalakshmi, L., RatnaKumari.G., et al. Isolation, Speciation and Antifungal Susceptibility Testing of Candida from Clinical Specimens at a Tertiary Care Hospital Sch. J. App. Med. Sci. 2014; 2(6):3193-3198.
19. Rizvi, M.W., Malik A., Shahid, M., Singhal, S. Candida albicans infections in a north Indian tertiary care hospital, antifungal resistance pattern and role of SDS-PAGE for characterization. Biology and Medicine. 2011;3(2):176-181.
20. Feglo P. K., Narkwa P. Prevalence and Antifungal Susceptibility Patterns of Yeast Isolates at the Komfo Anokye Teaching Hospital (KATH), Kumasi, British Microbiol Res J. 2012.2(1): 10-22.
21. Roy R., et al. Trend of Candida infection and antifungal resistance in a tertiary care hospital of north east India. African J. of Microbiol Res. June 2013;Vol. 7(24): 3112-16.
22. Kashid A.R., Belawadi S., Devi G. Characterization and antifungal susceptibility testing for Candida species in a tertiary care hospital. J.Health Sci. Res. 2011; 2(2):1-7.
23. Dalal P. J., Kelkar S.S. Clinical patterns of Candida infections in Bombay. Indian J Dermat Venerol Leprosy 1980; 46(1): 31-2.
24. Lal Binesh., Y Kalyani M., et al. Phenotypic Characterization of Candida species and their antifungal susceptibility from a tertiary care centre Tamil Nadu JPBMS ., 2011; 11 (12):1-5.
25. Vijaya D., Harsha T.R., Nagaratnamma, T. Candida speciation using chrom agar. J Clin and Diagnostic Res. 2011; 5: 755-757.
26. Shivanand D., Dominic, S. Species identification of Candida isolates in various clinical specimens with their antifungal susceptibility patterns. J of clinical and diagnostic research. 2011; 5(6):1177-81. [PubMed]
27. Pahwa N, Kumar R, Nirkhiwale S, Bandi A. Species distribution and drug susceptibility of candida in clinical isolates from a tertiary care centre at Indore. Indian J Med Microbiol. 2014 Jan-Mar;32(1):44-8. doi: 10.4103/0255-0857.124300. [PubMed]


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


