A prospective study of hidden cases of beta thalassemia trait in voluntary blood donors at tertiary care hospital of south Gujarat
Abstract
Background: Hemoglobinopathies represent a significant national health burden in India. The two most common causes of microcytic (MCV less than 80 fl) anemia are iron deficiency anemia and beta-thalassemia trait. In most of these cases a trial of iron treatment done but in populations where Thalassemia is common, like in India, this approach leads to unnecessary iron therapy / iron overload. Therefore the study has been done to detect hidden cases of beta thalassemia in voluntary blood donors with microcytosis.
Materials and Methods: Total 393 donor samples were analyzed for complete blood count, ESR and serum ferritin levels. Mentzer index was calculated by MCV/RBC count formula. HPLC test was done on 12samples with Mentzer index <13 for quantification of HbA2.
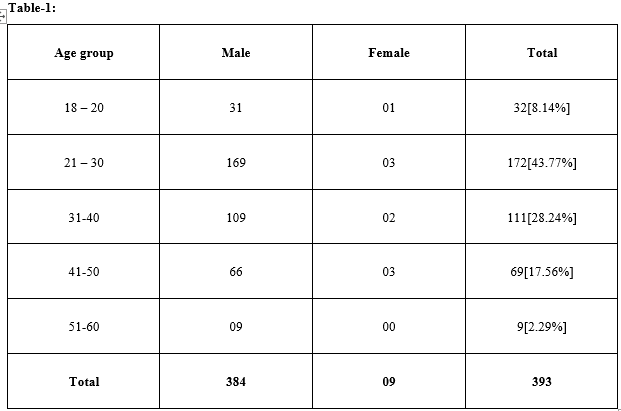
Results: Out of 393 blood donors, 384 were males and 9 were females. Low MCV detected in 58 samples [14.75%]. Out of 12 samples tested by HPLC, 6 cases were Beta thalassemia trait [1.53%], 5 were normal and one was? sickle cell trait/ ? Hb D trait. Out of 6 BTT cases, 3 cases show normal ferritin value, 2 with low ferritin level and one with high ferritin level.
Conclusions: The study revealed a high prevalence of IDA and BTT in blood donors and a higher probability of finding these in the microcytic samples. Screening for thalassemia trait by routine blood counts in all the blood donor samples and if required by HPLC, should be included in the standard blood testing policy after blood donation.
Downloads
References
2. Wonke B, Modell M, Marlow T, Khan M, Modell B. Microcytosis, iron deficiency and thalassaemia in a multi-ethnic community: a pilot study. Scand J Clin Lab Invest. 2007; 67(1): 87-95. doi:10.1080/00365510 6010 46474
3. Lukens JN. The thalassemias and related disorder: an overview. Wintrobe's Clinical Hematology. 1999:405-433
4. Sukumaran PK. Abnormal Hemoglobins in India. In: Sen NN, Basu AK, editors. Trends in Hematology. 1975. p. 225–261
5. Saran RK, Makroo RN. Transfusion Medicine Technical Manual, Directorate General of Health Services, Government of India, New Delhi. 1991
6. Krejcie RV, Morgan DW. Determining sample size for research activities. Educate Psychol Measure. 1970;30(3):607-610.
7. Pearson HA, O'Brien RT, McIntosh S. Screening for thalassemia trait by electronic measurement of mean corpuscular volume. N Engl J Med. 1973;288(7):351-353. doi:10.1056/NEJM197302152880706
8. Soliman AR, Kamal G, Walaa AE, Mohamed TS. Blood indices to differentiate between β-thalassemia trait and iron deficiency anemia in adult healthy Egyptian blood donors. Egypt J Haematol. 2014;39 (3): 91-97. doi: 10.4103/1110-1067.148223
9. Tiwari AK, Chandola I. Comparing prevalence of Iron Deficiency Anemia and Beta Thalassemia Trait in microcytic and non-microcytic blood donors: suggested algorithm for donor screening. Asian J Transfus Sci. 2009;3(2):99-102.
10. Lau YL, Chan LC, Chan YY, Ha SY, Yeung CY, Waye JS, et al. Prevalence and genotypes of alpha- and beta-thalassemia carriers in Hong Kong -- implications for population screening. N Engl J Med. 1997;336 (18):1298-1301. doi: 10.1056/ NEJM19970 5013361805
11. Massey AC. Microcytic anemia. Differential diagnosis and management of iron deficiency anemia. Med Clin North Am. 1992;76(3):549-566. doi: https:// doi.org/10.1016/S0025-7125(16)30339-X
12. Clark SF. Iron deficiency anemia. Nutr Clin Pract. 2008; 23 (2):128-141. doi: 10.1177/088453360 8314536.
13. Ou CN, Rognerud CL. Diagnosis of hemoglobin-pathies:electrophoresis vs. HPLC. Clin Chim Acta. 2001; 313(1-2):187-194. doi:10.1016/s0009-8981 (01) 00672-6
14. Clarke GM, Higgins TN. Laboratory investigation of hemoglobinopathies and thalassemias: review and update. Clin Chem. 2000;46(8 Pt 2):1284-1290.
15. Madan N, Sikka M, Sharma S, Rusia U. Frequency of coincident iron deficiency and beta-thalassaemia trait. J Clin Pathol. 1996;49(12):1021. doi: 10.1136/jcp.49.12.1021-b
16. Meena VK, Kumar K, Meena LP, Bharti A, Kumar A. Screening for Hemoglobinopathies in blood donors from eastern Uttar Pradesh. Natl J Med Res. 2012;2 (3):366-368.
17. Lisot CL, Silla LM. Screening for hemoglobin-pathies in blood donors from Caxias do Sul, Rio Grande do Sul, Brazil: prevalence in an Italian colony. Cad Saude Publica. 2004;20(6):1595-1601. Epub 2004. doi:/ S0102-311X2004000600017
18. Hershko C, Konijn AM, Loria A. Serum Ferritin and Mean Corpuscular Volume Measurement in the Diagnosis of β-Thalassaemia minor and Iron Deficiency. Acta haematologica. 1979;62(4):236-239. doi: 10.1159/000207578
19.Loria A, Konijn AM, Hershko C.Serum ferritin in beta-thalassemia trait. Isr J Med Sci. 1978;14(11):1127-1131.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


