Prevalence of acute undifferentiated febrile illnesses in a tertiary care centre in Telangana, South India
Abstract
Introduction: Increased incidence of acute undifferentiated febrile illnesses (AUFI) are observed with the beginning of monsoon season in tropical countries. Diverse aetiologies, overlapping clinical presentations and mixed infections complicate the diagnosis and management of febrile illnesses. Knowledge of the local aetiology and seasonal prevalence of these diseases would enable physicians and policy makers to take adequate control measures. Hence the present study was undertaken to understand the aetiology of AUFI and the prevalence of multiple infections in patients attending our tertiary care hospital in Telangana, South India.
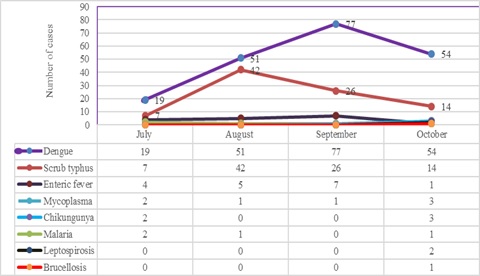
Material and Methods: A total of 932 patients presenting with AUFI over a period of four months from July to October 2018 were tested for various causes of fever by serological tests. Dengue, scrub typhus, Leptospira and Chikungunya were tested by rapid tests and ELISA. Latex agglutination kits were used for diagnosis of Salmonella and Brucella infections. Peripheral smear examination was used to diagnose malaria.
Results: Dengue was the most common infection seen in 21.6% of patients followed by scrub typhus in 9.5%. Peak incidence of Dengue was seen in the month of September and maximum scrub typhus cases were diagnosed in August. Dual infections were documented in 1.9% of patients; most common being dengue with scrub typhus.
Conclusion: Awareness of the local aetiology of AUFI guides clinicians in prioritising clinical and diagnostic workup and initiating appropriate empirical and supportive therapy. As incidence of multiple infections is increasing, comprehensive clinical and diagnostic exploration for probable pathogens need to be considered in treatment non-responsive AUFI patients.
Downloads
References
2. Chrispal A, Boorugu H, Gopinath KG, Chandy S, Prakash JA, Thomas EM, et al. Acute undifferentiated febrile illness in adult hospitalized patients: The disease spectrum and diagnostic predictors- An experience from a tertiary care hospital in South India. Trop Doct. 2010;40(4):230–234. doi: 10.1258/td.2010.100132.
3. Zeller H, Van Bortel W, Sudre B. Chikungunya: its history in Africa and Asia and its spread to new regions in 2013-2014. J Infect Dis. 2016;214(suppl 5):S436–S440. doi: https://doi.org/10.1093/infdis/jiw391
4. Selvaretnam A, Sahu PS, Sahu M, Ambu S. A review of concurrent infections of malaria and dengue in Asia. Asian Pac J Trop Biomed. 2016;6(7):633–638. doi: https://doi.org/10.1016/j.apjtb.2016.05.008
5. Basheer A, Iqbal N, Mookkappan S, Anitha P, Nair S, Kanungo R, et al. Clinical and laboratory characteristics of dengue-Orientia tsutsugamushi coinfection from a tertiary care center in South India. Mediterr J Hematol Infect Dis 2016;8(1):e2016028. doi: 10.4084/MJHID.2016.028.
6. Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, et al. Leptospirosis: a zoonotic disease of global importance. Lancet Infect Dis. 2003;3 (12):757–771. doi: https://doi.org/10.1016/S1473-3099 (03) 00830-2
7.Pradutkanchana J, Pradutkanchana S, Kemapanmanus M, Wuthipum N, Silpapojakul K. The etiology of acute pyrexia of unknown origin in children after a flood. Southeast Asian J Trop Med Public Health. 2003; 34(1):175-178.
8. Bruce MG, Sanders EJ, Leake JA, Zaidel O, Bragg SL, Aye T, et al. Leptospirosis among patients presenting with dengue-like illness in Puerto Rico. Acta Trop.2005;96(1):36–46.doi: 10.1016/j.actatropica.2005. 07.001
9. Levett PN, Branch SL, Edwards CN. Detection of dengue infection inpatients investigated for leptospirosis in Barbados. Am J Trop Med Hyg. 2000; 62(1):112–114.
10. Jena B, Prasad MNV, Murthy S. Demand pattern of medical emergency services for infectious diseases in Andhra Pradesh – A geo-spatial temporal analysis of fever cases. Indian Emerg J. 2010;1(5):821.
11. Murdoch DR, Woods CW, Zimmerman MD, Dull PM, Belbase RH, Keenan AJ, et al. The aetiology of febrile illness in adults presenting to Patan Hospital in Kathmandu, Nepal. Am J Trop Med Hyg. 2004;70(6): 670–675.
12. Sripanidkulchai R, Lumbiganon P. Aetiology of obscure fever in children at a university hospital in northeast Thailand. Southeast Asian J Trop Med Public Health. 2005;36(5):1243–1246.
13. Leelarasamee A, Chupaprawan C, Chenchittikul M, Udompanthurat S. Aetiologies of acute undifferentiated febrile illness in Thailand. J Med Assoc Thai. 2004; 87(5):464–472.
14. Ellis RD, Fukuda MM, McDaniel P, Welch K, Nisalak A, Murray CK, et al. Causes of fever in adults on the Thai-Myanmar border. Am J Trop Med Hyg. 2006; 74(1):108-113.
15. Gopalakrishnan S, Arumugam B, Kandasamy S, Rajendran S, Krishnan B. Acute undifferentiated febrile illness among adults - A hospital based observational study. J Evol Med Dent Sci. 2013; 2(14): 2305-2319.
16. Kashinkunti MD, Gundikeri SK, Dhananjaya M. Acute undifferentiated febrile illness- clinical spectrum and outcome from a tertiary care teaching hospital of north Karnataka. Int J Biol Med Res. 2013;4(2):3399-3402.
17. Mittal G, Ahmad S, Agarwal RK, Dhar M, Mittal M, Sharma S. Aetiologies of acute undifferentiated febrile illness in adult patients an experience from a tertiary care hospital in Northern India. J Clin Diagn Res 2015; 9(12):DC22–DC24. doi: 10.7860/JCDR/ 2015 / 11168.6990.
18. Rao PN, van Eijk AM, Choubey S, Ali SZ, Dash A, Barla P, et al. Dengue, chikungunya, and scrub typhus are important etiologies of non-malarial febrile illness in Rourkela, Odisha, India. BMC Infect Dis2019;19(1): 572. doi: 10.1186/s12879-019-4161-6.
19. Abhilash KP, Jeevan JA, Mitra S, Paul N, Murugan TP, Rangaraj A, et al. Acute Undifferentiated Febrile Illness in Patients Presenting to a Tertiary Care Hospital in South India: Clinical Spectrum and Outcome. J Glob Infect Dis 2016;8(4):147-154. doi: 10.4103/0974-777X. 192966
20. Shelke YP, Deotale VS, Maraskolhe DL. Spectrum of infections in acute febrile illness in central India. Indian J Med Microbiol. 2017;35(4):480-484. doi:10. 4103/ ijmm.IJMM_17_33.
21. Wangdi K, Kasturiaratchi K, Nery SV, Lau CL, Gray DJ, Clements ACA. Diversity of infectious aetiologies of acute undifferentiated febrile illnesses in south and Southeast Asia: a systematic review. BMC Infect Dis. 2019;19(1):577. doi: 10.1186/s12879-019-4185-y.
22. Morch K, Manoharan A, Chandy S, Chacko N, Alvarez-Uria G, Patil S, Henry A, Nesaraj J, Kuriakose C, Singh A, et al. Acute undifferentiated fever in India: a multicentre study of aetiology and diagnostic accuracy. BMC Infect Dis. 2017;17(1):665. doi: 10. 1186/ s12879-017-2764-3.
23. Raina S, Raina RK, Agarwala N, Raina SK, Sharma R. Coinfections as an aetiology of acute undifferentiated febrile illness among adult patients in the sub-Himalayan region of North India. J Vector Borne Dis 2018;55(2):130–136. doi: 10.4103/0972-9062.242560.
24. Prasad N, Murdoch DR, Reyburn H, Crump JA. Etiology of severe febrile illness in low-and middle-income countries: a systematic review. PLoS One. 2015;10(6): e0127962. doi: 10.1371/journal.pone. 012 7962.
25. Aung AK, Spelman DW, Murray RJ, Graves S. Rickettsial infections in Southeast Asia:implications for local populace and febrile returned travellers. Am J Trop Med Hyg. 2014;91(3):451–460. doi: 10.4269/ ajtmh.14-0191.
26. Suresh V, Krishna V, Raju CHN, Teja PS, Usha V. A rare case of triple infection with dengue, malaria and typhoid. Int J Res Dev Health. 2013;1(4):200-203.
27. Singhsilarak T, Phongtananant S, Jenjittikul M, Watt G, Tangpakdee N, Popak N, et al. Possible acute coinfections in thai malaria patients. Southeast Asian J Trop Med Public Health. 2006;37(1):1-4.
28. Sharma A, Raina R, Dhiman P, Adarsh, Madhabhavi I, Panda P. Rare Coinfection of Scrub Typhus and Malaria in Immunocompetent Person. Online J Health Allied Scs. 2012;11(2):12.
29. Ahmad S, Dhar M, Mittal G, Bhat NK, Shirazi N, Kalra V, et al. A comparative hospital-based observational study of mono and co-infections of malaria, dengue virus and scrub typhus causing acute undifferentiated fever. Eur J Clin Microbiol Infect Dis. 2016;35(4):705–711. doi: 10.1007/s10096-016-2590-3.
30. Iqbal N, Viswanathan S, Remalayam B, Muthu V, George T. Pancreatitis and MODS Due to Scrub Typhus and Dengue Co-Infection. Trop Med Health. 2012;40 (1):19–21. doi: 10.2149/tmh.2012-07.
31. Chahar HS, Bharaj P, Dar L, Guleria R, Kabra SK, Broorl S. Coinfections with chikungunya virus and Dengue virus in Delhi,India. Emerg Infect Dis. 2009; 15(7):1077–1080. doi: 10.3201/eid1507.080638.
32. Londhey V, Agrawal S, Vaidya N, Kini S, Shastri JS, Sunil S. Dengue and chikungunya coinfections: The inside story. J Assoc Physicians India. 2016; 64(3):36–40.
33. Suttinont C, Losuwanaluk K, Niwatayakul K, Hoontrakul S, Intaranongpai W, Silpasakorn S, et al. Causes of acute, undifferentiated, febrile illness in rural Thailand: Results of a prospective observational study. Ann Trop Med Parasitol 2006;100(4):363–370.
34. Mueller TC, Siv S, Khim N, Kim S, Fleischmann E, Ariey F, et al. Acute undifferentiated febrile illness in rural Cambodia: A 3-year prospective observational study. PLoS One2014;9(4):e95868. doi: 10.1371/ journal. pone.0095868.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


