Serum procalcitonin as diagnostic marker for postoperative surgical wound infection
Abstract
Background: Early diagnosis and treatment of postoperative infections is important to curtail the morbidity and economic burden associated with them. Currently there is no reliable diagnostic markers to differentiate infectious cause of postoperative fever from non-infectious one. The effectiveness of serum procalcitonin in establishing the same was investigated.
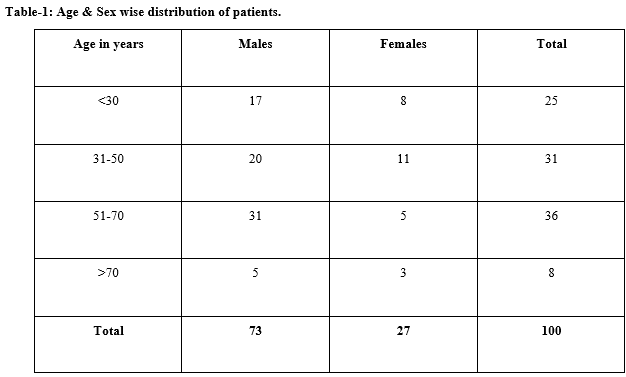
Method: It was a cross-sectional study in which 100 consecutive patients who had onset of fever within seven days of the surgery were evaluated. These patients were divided into two groups of 50 each. Group A comprised of 50 patients having fever and elevated TLC (total leukocyte count) & ANC (absolute neutrophil count). Group B had 50 patients having fever but with normal TLC and ANC. All patients were assessed for C-reactive protein level, and serum procalcitonin and wound condition. Patients who had unhealthy wounds, their wound swabs were sent for microbiological work up.
Results: 11/50 patients had raised serum procalcitonin levels in group A whereas in group B none had abnormal PCT levels. The statistical analysis showed that this difference was statistically significant as p value was <0.05. There was also statistically significant relation between PCT and wound condition. All patients with unhealthy wound were culture positive and also had raised raised serum procalcitonin levels. However, CRP was raise in patients in both the groups (96/100) which was found to be statistically insignificant with P value =0.307.
Conclusion: Serum procalcitonin is a helpful biomarker marker in differentiating infectious from noninfectious causes of postoperative fever and can be used as an adjunct with clinical and microbiological findings.
Downloads
References
Hunziker S, Hügle T, Schuchardt K, Groeschl I, Schuetz P, Mueller B, et al. The value of serum procalcitonin level for differentiation of infectious from noninfectious causes of fever after orthopaedic surgery. J Bone Joint Surg Am. 2010;92(1):138-148.doi: 10. 2106/ JBJS.H.01600
Doharty G. M., Way L.W.,editors. Current Surgical Diagnosis and Treatment. 12thed. New York: McGraw Hill; 2006. p.106-107.
Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis. 2004; 39(2): 206-17. doi:10.1086/421997
Black S, Kushner I, Samols D. C-reactive Protein. J Biol Chem. 2004;279(47):48487-48490. doi:10.1074/ jbc. R400025200
Baumann H, Gauldie J. The acute phase response. Immunol Today. 1994;15(2):74-80. doi:10.1016/0167-5699 (94)90137-6
Rowther FB, Rodrigues CS, Deshmukh MS, Kapadia FN, Hegde A, Mehta AP, et al. Prospective comparison of eubacterial PCR and measurement of procalcitonin levels with blood culture for diagnosing septicemia in intensive care unit patients. J Clin Microbiol. 2009; 47 (9):2964-2969. doi: 10.1128/JCM.00418-07. Epub 2009 Jul 29.
Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, et al. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994;79(6):1605-1608. doi:10.1210/ jcem. 79.6.7989463
Saltzman BM, Mayo BC, Bohl DD, Frank RM, Cole BJ, Verma NN, et al. Evaluation of fever in the immediate post-operative period following shoulder arthroplasty. Bone Joint J. 2017;99-B(11):1515-1519. doi: 10.1302/0301-620X.99B11.BJJ-2017-0469.R1.
Procedures for the Collection of Diagnostic Blood Specimens by Venipuncture; Approved Standard—Fifth Edition. NCCLS document H3-A5 [ISBN 1-56238-515-1]. NCCLS, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898 USA, 2003
Cheesbrough M. District laboratory practice in tropical countries. Cambridge university press; 2006.
Clinical and Laboratory Standards Institute (CLSI): Performance standards for antimicrobial susceptibility testing. 2014; 24th ed.
Galicier C, Richet H. A prospective study of postoperative fever in a general surgery department. Infect Control. 1985;6(12):487-490.
Laffey JG, Boylan JF, Cheng DC. The systemic inflammatory response to cardiac surgery: implications for the anesthesiologist. Anesthesiol. 2002;97(1):215-252. doi:10.1097/00000542-200207000-00030
Schey D, Salom EM, Papadia A, Penalver M. Extensive fever workup produces low yield in deter-mining infectious etiology. Am J Obstet Gynecol. 2005; 192(5):1729-1734.DOI:10.1016/j.ajog.2004.11.049
BalcI C, Sungurtekin H, Gürses E, Sungurtekin U, Kaptanoglu B. Usefulness of procalcitonin for diagnosis of sepsis in the intensive care unit. Crit Care. 2003; 7(1):85-90. doi: 10.1186/cc1843Epub 2002 Oct 30.
Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C, et al. Use of procalcitonin to reduce patients' exposure to antibiotics in intensive care units (PRORATA trial): a multicentrerandomised controlled trial. Lancet. 2010;375(9713):463-474. doi: 10.1016/ S0140-6736(09)61879-1. Epub 2010 Jan 25.
Lee GM, Harper MB. Risk of bacteremia for febrile young children in the post-Haemophilus influenzae type b era. Arch Pediatr Adolesc Med. 1998;152(7):624-8.doi:10.1001/archpedi.152.7.624
Kraft CN, Krüger T, Westhoff J, Lüring C, Weber O, Wirtz DC, et al. CRP and leukocyte-count after lumbar spine surgery: fusion vs. nucleotomy. Acta Orthop. 2011; 82(4): 489-493.doi: 10.3109/17453674.2011. 588854. Epub 2011 Jun 10.
Hu L, Shi Q, Shi M, Liu R, Wang C. Diagnostic Value of PCT and CRP for Detecting Serious Bacterial Infections in Patients With Fever of Unknown Origin: A Systematic Review and Meta-analysis.Appl Immuno-histochem Mol Morphol. 2017; 25(8):e61-e69. doi: 10. 1097/PAI.0000000000000552.
Chirouze C, Schuhmacher H, Rabaud C, Gil H, Khayat N, Estavoyer JM, et a. Low serum procal-citonin level accurately predicts the absence of bacteremia in adult patients with acute fever. Clin Infect Dis. 2002; 35(2):156-161. Epub 2002 Jun 17. doi:10. 1086/ 341023.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


