Hematological study of iron deficiency anemia and β thalassemia trait in Sindhi community of Bundelkhand region of Madhya Pradesh with predictive value of red cell indices to discriminate them
Abstract
Background: Ethnic groups like Sindhis, Kutchis, Lohanas, Punjabis, few Muslim groups as well as few tribal populations have higher prevalence of hemoglobinopathy esespecially β thalassemia carriers. β Thalassemia traits are commonly misdiagnosed as iron deficiency anemia. Red cell indices are helpful to discriminate anemia and to detect subjects who have high probability of requiring appropriate follow up and to reduce unnecessary investigation cost.
Aims and objectives: 1) To study red blood cell indices in all cases of microcytic hypochromic anemia. 2) Estimation of HbA2 levels and serum ferritin levels to confirmiron deficiency anemia and β thalassemia trait. 3) To evaluate the diagnostic values of various red cell indices in discriminating iron deficiency anemia and β thalassemia trait.
Materials and methods: It is a prospective observation study carried out on Sindhi individuals of Sagar District of Bundelkhand region of Madhya Pradesh. Hemoglobin, RBC count, MCV, MCH and RDW were determined. Serum ferritin levels and HbA2 levels were detected.
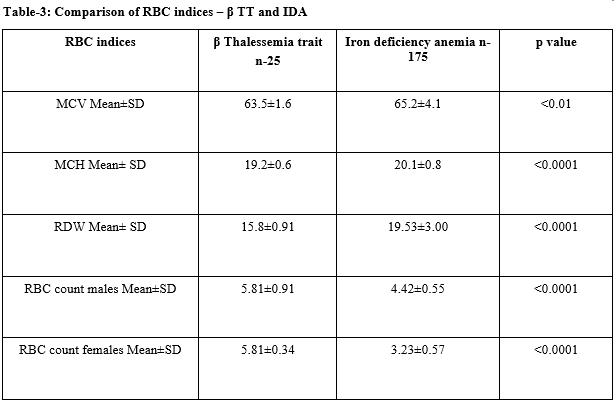
Result: Out of total 200 cases of Sindhi individuals 25 patients (12.5%) were grouped in β thalassemia trait while 175 patients (87.5%) were grouped in iron deficiency anemia group on the basis of HbA2 and serum ferritin level. Significant difference was found inmean MCV, MCH, RDW and RBC count and showed high sensitivity and specificity to discriminate iron deficiency anemia from β thalassemia.
Conclusion: Sindhi community of Sagar district of Madhya Pradesh showed high prevalence of β thalassemia trait. Mass awareness and proper pre marriage genetic counseling and prenatal diagnosis should be done to reduce the burden of disease.
Downloads
References
2. Singh M, Gautam A. To evaluate anaemia by erythrocyte indices, red cell distribution width and haemoglobin electrophoresis with special reference to thalassemia in paediatric age group. J Evol Med Dent Sci. 2015;4(11):1755-64.
3. Angastiniotis M, Modell B. Global epidemiology of hemoglobin disorders. Ann N Y Acad Sci. 1998;850: 251-69. DOI:10.1111/j.1749-6632.1998.tb10482.x
4. Kandhro AH, Prachayasittikul V, Isarankura Na-Ayudhya C, Nuchnoi P. Prevalence of Thalassemia Traits and Iron Deficiency Anemia in Sindh, Pakistan. Hemoglobin. 2017;41(3): 157-163. DOI: 10.1080/ 03630269. 2017.1345759. Epub 2017.
5. Cao A, Kan YW. The prevention of thalassemia. Cold Spring HarbPerspect Med. 2013;3(2):a011775. DOI: 10.1101/cshperspect.a011775.
6. Vehapoglu A, Ozgurhan G, Demir AD, UzunerS, Nursoy MA, Turkmen S et al. Hematological indices for differential diagnosis of Beta thalassemia trait and iron deficiency anemia. Anemia. 2014;2014. DOI: http://dx.doi.org/10.1155/2014/576738
7.Jameel T, Baig M, Ahmed I, Hussain MB, Alkhamaly MBD. Differentiation of beta thalassemia trait from iron deficiency anemia by hematological indices. Pak J Med Sci. 2017; 33(3): 665-669. DOI: 10.12669/pjms. 333. 12098.
8. Urrechaga E, Borque L, Escanero JF. The role of automated measurement of RBC subpopulations in differential diagnosis of microcytic anemia and β-thalassemia screening. Am J Clin Pathol. 2011;135 (3):374-9. DOI: 10.1309/AJCPJRH1I0XTNFGA.
9. Rathod DA, Kaur A, Patel V, Patel K, Kabrawala R, Patel V, et al. Usefulness of cell counter-based parameters and formulas in detection of beta-thalassemia trait in areas of high prevalence. Am J Clin Pathol. 2007;128(4):585-9. DOI:10.1309/R1YL4 B4BT 2 WCQDGV
10. Colah RB. Strategies for prevention of thalassemia and hemoglobinopathies. J Assoc Physicians India. 1994;42(10):810-4.
11. Rakholia R, Chaturvedi P. Prevalence of β thalassemia carrier state in Sindhi community of Wardha and evaluation of risk factors for β thalassemia trait. Niger J Clin Pract. 2013;16(3):375-80. DOI: 10. 4103/ 1119-3077.113468.
12. Sirdah M, Tarazi I, Al Najjar E, Al Haddad R. Evaluation of the diagnostic reliability of different RBC indices and formulas in the differentiation of the beta-thalassaemia minor from iron deficiency in Palestinian population. Int J Lab Hematol. 2008;30(4):324-330. DOI: 10.1111/j.1751-553X.2007.00966.x.
13. Jaswani P, Nigam RK, Kothari S. Clinico-haematological study of iron deficiency anaemia and b-thalassemia traitpredictive value of Sehgal index and various complete blood count indices to discriminate between iron deficiency anaemia and b-thalassemia trait and confirmation using haemoglobin electrophoresis/ HPLC. J Evol Med Dent Sci. 2018;7(17):2118-25.
14. Soliman AR, Kamal G, Walaa AE, Mohamed TS. Blood indices to differentiate between β-thalassemia trait and iron deficiency anemia in adult healthy Egyptian blood donors. Egypt J Haematol. 2014;39(3): 91. DOI: 10.4103/1110-1067.148223
15. Reema B, Shailaja S, Divyanshu S, Ss T, Sunita S. Reliability of Different RBC Indices to Differentiate Between Beta Thalassemia Trait and Iron Deficiency Anemia During Antenatal Screening, World J Pathol, 2018; 7(3):14-20.
16. Jassim AN. Comparative behavior of red blood cells indices in iron deficiency anemia and β-thalassemia trait. Iraqi J Hematol. 2016 1;5(2):183.DOI: 10.4103/ 2072-8069.198129


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


