Intestinal parasitic infections in patients attending a tertiary care centre
Abstract
Introduction: Intestinal parasitic infections are prevalent worldwide with a range of 11- 90% in developing countries like India. The clinical presentations vary from self-limiting diarrhea in immunocompetent patients to profuse diarrhea in immmunocompromised individuals.
Objectives: To determine the prevalence of intestinal parasites in patients presenting with diarrhea.
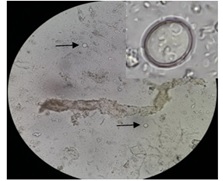
Material and Methods: Stool specimens from patients with diarrhea were received in the department of Microbiology, G.I.P.M.E.R during 6 months duration from September 2017 to March 2018. All specimens were examined grossly for the color, consistency and presence of any visible adult worms or their segments. Microscopic examination was done by direct saline/iodine wet mount. The specimens from immunocompromised patients were subjected to Formol-ether concentration technique and Modified Ziehl Neelson’s stain.
Results: Total 57 stool specimens were received from 34 female and 23 male diarrheic patients. Majority of cases were in the 31-40 years age group. Intestinal parasites were detected in 10 specimens, out of whom 7 were Protozoa and 3 were Helminths. Over all, Cryptosporidium oocysts were the most common. Among the 10 positive cases, 7 were immunocompromised with 4 cases of AIDS/HIV, 2 of Ulcerative colitis and one case with Myasthenia gravis and Diabetes mellitus.
Conclusion: The prevalence of parasitic infections indicates the socioeconomic status of the society. Recently many studies across India have reported protozoa to be common than the other intestinal parasites. The preponderance of coccidians in the present study highlights the importance of aggressive screening of these parasites, especially in immunocompromised group of patients.
Downloads
References
2. Rituparna B, Bhattacharya P, Paul UK, Bandyo-padhyay A.Nitin S, Venkatesh V, Husain N, Masood J, Agarwal GG. Overview of intestinal parasitic prevalence in rural and urban population in Lucknow, north India. J Commun Dis. Dec;39(4):217-23. PubMed PMID: 18697590.
3. Kumar S, Nag VL, Dash S, Maurya AK, Hada V, Agrawal R, Narula H, Sharma A. Spectrum of parasitic infections in patients with diarrhea attending a tertiary care Hospital in western Rajasthan, India. J Clin Diagn Res. 2017Aug;11(8):DC01-DC04.DOI: 10.7860/ JCDR / 2017/ 29001.10346.
4. Bora I, Dutta V, Lyngdoh WV, Khyriem AB, Durairaj E, Phukan AC. Study of intestinal parasites among the immunosuppressed patients attending a tertiary-care center in Northeast India.IJMSPH 2016;5 (5):924-929. DOI:10.5455/ijmsph.2016. 08012016327
5. Manochitra K, Padukone S, Phillips SA, Parija SC. Prevalence of intestinal parasites among patients attending a tertiary care centre in South India. Int. J. Curr. Microbiol. App. Sci 2016 Sep; 5(9):190-197. DOI: http://dx.doi.org/10.20546/ijcmas.2016.509.021
6.Cama VA, Mathison BA.Infections by Intestinal coccidian and Giardia duodenalis. Clin Lab Med. 2015 Jun; 35 (2): 423-44. DOI: 10. 1016/j. cll. 2015. 02.010.
7. Tzipori S, Ward H. Cryptosporidiasis: biology, pathogenesis and disease. Microbes and Infection 2002; 4: 1047–1058.
8. Al-Megrin WA. Intestinal parasites infection among immunocompromised patients in Riyadh, Saudi Arabia. Pak J Biol Sci. 2010 Apr 15;13(8):390-4. DOI: 10. 3923/ pjbs. 2010.390.394
9. Kamki Y, Singh R, Singh N, Lungram P, Singh B. Intestinal protozoal and helminthic infections in immunocompromised patients attending RIMS Hospital, Imphal. Journal of Medical Society 2015 Aug; 29 (2): 74-78. DOI: 10.4103/ 0972-4958. 163192.
10. Mathuria YP, Singh A. Prevalence of Intestinal Parasites at a Tertiary Care Centre at Moradabad, Western Uttar Pradesh, India: A One-Year Obser-vational Study. Ann. Int. Med. Den. Res. 2017; 3(5): 7-10. DOI:10.21276/aimdr. 2017.3.5.MB2
11. Dudeja M, Nandy S, Das AK,Alam S, Tiwari R. Prevalence of Intestinal Parasites in Slum Areas of Southern Delhi. Int. J. Microbiol. Res. 2012 Sep;4 (8): 312-315.
12. Choubisa SL, Jaroli VJ, Choubisa P, Mogra N. Intestinal parasitic infection in Bhil tribe of Rajasthan, India. J Parasit Dis. 2012 Oct;36(2):143-8. DOI: 10. 1007/ s12639-012-0151-y
13. Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, Jacobson J. Helminth infections: the great neglected tropical diseases. J Clin Invest. 2008 May; 118 (4):1311-21. DOI: 10.1172/JCI34261
14. Jacobsen KH, Ribeiro PS, Quist BK, Rydbeck BV. Prevalence of intestinal parasites in young Quichua children in the highlands of rural Ecuador. J Health Popul Nutr 2007 Dec;25:399-405. Pub Med PMID: 18402182; PubMed Central PMCID: PMC 2754013.
15. Nitin S, Venkatesh V,Husain N, Masood J, Agarwal G. J Commun Dis. Overview of intestinal parasitic revalence in rural and urban population in Lucknow, north India.2007 Dec;39(4):217-23. PubMed PMID: 18697590.
16. Kaur R, Rawat D, Kakkar M, Uppal B, Sharma VK. Intestinal parasites in children with diarrhea in Delhi, India. Southeast Asian J Trop Med Public Health. 2002 Dec; 33(4):725-9. PubMed PMID: 12757217.
17. Maha Bouzid, Paul R. Hunter, Rachel M. Chalmers, Kevin M. Tyler. Cryptosporidium Pathogenicity and Virulence. Clinical Microbiology Reviews 2013;26(1): 115-134. DOI: 10.1128/CMR.00076-12
18. Salam N, Azam S.Prevalence and distribution of soil transmitted helminthes in India.BMC Public Health 2017 Feb;17:201. DOI: https://doi.org/10.1186/s12889-017-4113-2
19. Vanathy K, Parija SC, Mandal J, Hamide A, Krishnamurthy S. Detection of Cryptosporidium in stool samples of immunocompromised patients. Trop Parasitol. 2017 Jun;7(1):41-46. DOI: 10.4103/tp.TP_ 66_16.
20. Kumar S S, Ananthan S, Lakshmi P. Intestinal parasitic infection in HIV infected patients with diarrhoea in Chennai. Indian J Med Microbiol 2002 Apr-Jun;20(2):88-91. PubMed PMID: 17657039.
21.Banerjee D, Deb R, Dar L, Mirdha BR, Pati SK, Thareja S, Falodia S, Ahuja V.High frequency of parasitic and viral stool pathogens in patients with active ulcerative colitis: report from a tropical country. Scand J Gastroenterol. 2009;44(3):325-31. DOI: 10. 1080/ 00365520802556809.
22. Vadlamudi N, Maclin J, Dimmitt RA, Thame KA. Cryptosporidial infection in children with inflammatory bowel disease.J Crohns Colitis. 2013 Oct;7(9):e337-43. DOI: 10.1016/j.crohns.2013.01.015
23. Yamamoto-Furusho J.K. Torijano-Carrera E. Intestinal protozoa infections among patients with Ulcerative colitis: Prevalence and impact on clinical disease course. Digestion 2010;82(1):18-23. DOI: 10. 1159/ 000273871.
24. Yu Zhen, Lin Liao, and Hu Zhang. Intestinal Giardiasis Disguised as Ulcerative Colitis. Case Reports in Gastrointestinal Medicine 2018. DOI: https://doi.org/ 10.1155/2018/8968976 Article ID 8968976.
25. Saraei M, Hosseinbigi B, Shahnazi M, Bijani B. Fatal Strongyloides hyper-infection in a patient with myasthenia gravis. Infection. 2014 Dec;42(6):1039-42. DOI: 10.1007/s15010-014-0637-x
26. Raúl Romero-Cabello, Javier Villagroy Gómez, Mercedes Hernández González,Raúl Romero Feregrino. Hyperinfection with Strongyloides stercoralis BMJ Case Rep 2012: bcr 2012006819. doi: 10.1136/bcr-2012- 006819
27. Sharifdini M, Hesari A, Mahdavi SA, Alipour A, Kia EB. Strongyloides stercoralis hyperinfection in an unconscious diabetic patient with dermatomyositis. Indian J Pathol Microbiol 2018 Jan-Mar;61(1):109-12. DOI: 10.4103/IJPM.IJPM_734_16.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


