Characterisation of Acinetobacter with special reference to carbapenem resistance and biofilm formation
Abstract
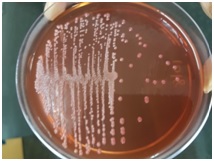
Background: Acinetobacter species cause hospital outbreaks and are often multidrug resistant. A wide range of resistance determinants make them successful nosocomial pathogens. In the present study, authors have identified and speciated Acinetobacter from various clinical specimens by a simplified phenotypic identification scheme determined their antibiotic susceptibility pattern focussing on Carbapenem resistance and have also evaluated their biofilm producing ability.
Method: Clinical samples were screened for Acinetobacter species and isolates were speciated. Antibiogram was determined by performing Kirby-Bauer disc diffusion method. Isolates resistant to Carbapenems were subjected to Modified Hodge Test (MHT) and Meropenem-EDTA Combined Disc Test (CDT). These isolates were further evaluated for their biofilm forming ability by the Microtitre Plate Method.
Results: Out of 174 isolates, the species most frequently isolated was Acinetobacter calcoaceticus-baumannii complex (ACB) (89.1%). 70.1% isolates were resistant to Carbapenems, of which 45.1% were MHT positive and 73.8% were CDT positive. 63.7% of the isolates were biofilm producers.
Conclusion: Simple identification schemes and antimicrobial susceptibility testing are cost effective and require fewer resources. Screening for Carbapenem resistance can help avoid unnecessary use of broad-spectrum antibiotics and thereby prevent treatment failure. Biofilms lead to decreased penetrability of antibiotics and make managing infections a clinical challenge. Further research is required to have a better understanding of the mechanism of biofilm formation and its implication in drug resistance.
Downloads
References
2. Mindolli PB, Salmani MP, Vishwanath G, Hanumanthapa AR. Identification and speciation of Acinetobacter and their antimimicrobial susceptibility testing. Al Ameen J Med Sci. 2010;3:3459.
3. Salmani MP, Mindolli PB. Speciation and Antimicrobial Susceptibility Pattern of Acinetobacter from Clinical Isolates in a Tertiary Care Centre. 2015;4(10):973–976.
4. Perez F, Hujer AM, Hujer KM, et al. Global challenge of multidrug-resistant Acinetobacter baumannii. Antimicrob Agents Chemother. 2007; 51(10):3471-84.[pubmed]
5. Bergogne-Berezin E, Friedman H, Bendinelli M, editors. Acinetobacter Biology and Pathogenesis: Springer; New York 2008.
6. Bergogne-Bérézin E, Towner KJ. Acinetobacter spp. as nosocomial pathogens: microbiological, clinical, and epidemiological features. ClinMicrobiol Rev. 1996; 9(2):148-65.[pubmed]
7. Vaneechoutte M, Dijkshoorn L, Nemec A, Kämpfer P, Wauters G. Acinetobacter, Chryseobacterium, Moraxella, and Other Nonfermentative Gram-Negative Rods. In: Versalovic J, Carroll K, Funke G, Jorgensen J, Landry M, Warnock D (editors). Manual of Clinical Microbiology, 10th Edition. ASM Press; Washington 2011: 714-738.
8. Towner KJ. Clinical importance and antibiotic resistance of Acinetobacter spp. Proceedings of a symposium held on 4-5 November 1996 at Eilat, Israel. J Med Microbiol. 1997;46(9):721-46. DOI:10.1099/00222615-46-9-721
9. European Centre for Disease Prevention and Control. Rapid risk assessment: Carbapenem- resistant Enterobacteriaceae. ECDC: 2016. Available from: http://ecdc.europa.eu/en/publications /Publications /carbapenem-resistant-enterobacteriaceae-risk-assessment-april-2016.pdf
10. Rodríguez-Baño J, Martí S, Soto S, et al. Biofilm formation in Acinetobacter baumannii: associated features and clinical implications. ClinMicrobiol Infect. 2008;14(3):276-8. DOI: 10.1111/j.1469-0691.2007.01916.x. Epub 2008 Jan 10.[pubmed]
11. Collee JG, Duguid JP, Fraser AG, Marmion BP, Simmons A. Laboratory strategy in the diagnosis of infective syndromes. In Collee JG, Marmion BP, Fraser AG, Simmons A. Editors. Mackie and McCartney practical medical microbiology.14th ed. New York; Church Livingstone publication; 1996: 53-94.
12. The Nonfermentative Gram-Negative Bacilli. In: Winn W, Allen S, Janda W, Koneman E, Procop G, Schreckenberger P, et al, editors. Colour Atlas and Textbook of Diagnostic Microbiology, 6th edition: Lippincott, Williams and Wilkins Publications; Philadelphia, USA 2006: 353-355
13. CLSI. 2015. Performance standards for antimicrobial susceptibility testing; twenty-second informational supplements. CLSI document M100-S25. Wayne PA: Clinical and Laboratory Standards Institute.
14. Sivasankari S, Senthamarai , Anitha C, Sastry A, Bhatt S, Kumudhavathi M S, et al. Phenotypic detection of carbapenem resistance in clinical isolates of Acinetobacter baumanii in Kanchipuram. Int J Appl Biol Pharm Technol 2014;5(1):50-53.
15. Modified Hodge Test for carbapenemase detection in Enterobacteriaceae. www.cdc.gov/HAI/pdfs/labSettings/HodgeTest_Carbapenemase_Enterobacteriaceae
16. Agrawal R, Sumana MN, Kishore A, Kulkarni M. Simple Method for Detection of Metallo – β–Lactamase Among Gram Negative Isolates. Online J Health Allied Sci. 2015;14(3):6.
17. Badave GK, Kulkarni D. Biofilm Producing Multidrug Resistant Acinetobacter baumannii: An Emerging Challenge. J Clin Diagn Res. 2015;9(1):DC08-10. DOI: 10.7860/JCDR/2015/11014.5398.[pubmed]
18. Raina D, Sharma N, Mahawal BS, Khanduri A, Pandita A. Speciation and antibiotic resistance pattern of Acinetobacter species in a tertiary care hospital in Uttarakhand. International Journal of Medical Research & Health Sciences 2016; 5(4): 89-96.
19. Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD et al. International study of the prevalence and outcomes of infection in intensive care units.JAMA. 2009;302(21):2323-9. DOI: 10.1001/jama.2009.1754.[pubmed]
20. Lee SO, Kim NJ, Choi SH, Kim TH, Chung JW, Woo JH, et al. Risk factors for acquisition of imipenem-resistant Acinetobacter baumannii: a case-control study. Antimicrob Agents Chemother. 2004; 48(1):224-8. DOI:10.1128/aac.48.1.224-228.2004.[pubmed]
21. Lone R, Shah A, Kadri SM, Lone S, Faisal S. Nosocomial multi-drug-resistant Acinetobacter infections – Clinical findings, risk factors and demographic characteristics. Bangladesh J Med Microbiol. 2009;3(01) 34-38.
22. Lahiri K, Mani NS, Purai SS. Acinetobacter species as nosocomial pathogen: Clinical significance and antimicrobial sensitivity. Med J Armed Forces India. 2004;60(1):7-10.
23. Oberoi A, Aggarwal A, Lal M. A decade of an underestimated nosocomal pathogen- Acinetobacter in a tertiary care hospital in Punjab. JK Science 2009; 11(1):24-26.
24. Singla P, Sikka R, Deep A, Seema, Chaudhary U. Pattern of antimicrobial resistance in clinical isolates of Acinetobacter species at a tertiary level health care facility in northern India. J Evol Med Dental Sci 2013;2(2):159-165.
25. Joshi SG, Litake GM, Satpute MG, Telang NV, Ghole VS, Niphadkar KB. Clinical and demographic features of infections caused by Acinetobacter species. Indian J Med Sci 2006;60(9):357-360.
26. Taneja N, Singh G, Singh M, Sharma M. Emergence of tigecycline &colistin resistant Acinetobacter baumanii in patients with complicated urinary tract infections in north India. Indian J Med Res. 2011;133:681-4.[pubmed]
27. Shareek PS, Sureshkumar D, Ramgopalakrishnan,Ramasubramanian V, Ghafur K, Thirunarayanan MA. Antibiotic Sensitivity Pattern of Blood Isolates of Acinetobacter species in a Tertiary Care Hospital: A Retrospective Analysis. Am. J. Infect. Dis. 2012;8(1):65-69.
28. Jaggi N, Sissodia P and Sharma L. Acinetobacter baumannii isolates: Epidemiology, antibiogram and nosocomial status studied over a 25 month period in a tertiary care hospital in India. Proceedings of the International Conference on Prevention and Infection Control, Jun. 29-Jul. 2, Geneva, Switzerland. 2011.
29. Prashanth K, Badrinath S. In vitro susceptibility pattern of Acinetobacter species to commonly used cephalosporins, quinolones, and aminoglycosides. Indian J Med Microbiol. 2004;22(2):97-103.[pubmed]
30. Amudhan SM, Sekar U, Arunagiri K, Sekar B. OXA beta-lactamase-mediated carbapenem resistance in Acinetobacter baumannii. Indian J Med Microbiol. 2011; 29(3):269-74. DOI: 10.4103/0255-0857.83911.[pubmed]
31. Shivaprasad A, Antony B, Shenoy P. Comparative evaluation of four phenotypic tests for detection of metallo-beta-lactamase and carbapenemase production in Acinetobacter baumannii. J Clin Diagn Res. 2014; 8(5):DC05–DC08. DOI: 10.7860/JCDR/2014/6447.4317
32. Irfan S, Zafar A, Guhar D, Ahsan T, Hasan R. Metallo-beta-lactamase-producing clinical isolates of Acinetobacter species and Pseudomonas aeruginosa from intensive care unit patients of a tertiary care hospital. Indian J Med Microbiol. 2008;26(3):243-5. DOI: 10.4103/0255-0857.42035.[pubmed]
33. John S, Balagurunathan R. Metallo beta lactamase producing Pseudomonas aeruginosa and Acinetobacter baumannii. Indian J Med Microbiol. 2011;29(3):302-4. DOI: 10.4103/0255-0857.83918.[pubmed]
34. Das NK, Grover N, Sriram R, Kumar M, Dudhat VL, Prasanna S. Prevalence of Carbapenem Resistance and Comparison between Different Phenotypic Methods for Detection of Metallo-Β-Lactamases in Gram Negative Non-Fermentative Bacteria in the Acute Wards of a Tertiary Care Centre. Int J Curr Microbiol App Sci 2016; 5(5):109-119. DOI: http://dx.doi.org/10.20546/ijcmas.2016.505.012
35. Manchanda V, Sanchaita S, Singh N. Multidrug resistant acinetobacter. J Glob Infect Dis. 2010;2(3):291-304. DOI: 10.4103/0974-777X.68538.[pubmed]
36. Bala M, Gupte S, Aggarwal P, Kaur M, Manhas A. Biofilm producing multidrug resistant Acinetobacter species from a tertiary care hospital : a therapeutic challenge. 2016; 4(7):3024–6. DOI: http://dx.doi.org/10.18203/2320-6012.ijrms20161997
37. Rodríguez-Baño J, Martí S, Soto S, et al. Biofilm formation in Acinetobacter baumannii: associated features and clinical implications. ClinMicrobiol Infect. 2008; 14(3):276-8. DOI: 10.1111/j.1469-0691.2007.01916.x. Epub 2008 Jan 10.[pubmed]
38. Rao RS, Karthika RU, Singh SP, et al. Correlation between biofilm production and multiple drug resistance in imipenem resistant clinical isolates of Acinetobacter baumannii. Indian J Med Microbiol. 2008;26(4):333-7. DOI: 10.4103/0255-0857.43566
39. Abdi-Ali A, Hendiani S, Mohammadi P, Gharavi S. Assessment of biofilm formation and resistance to imipenem and ciprofloxacin among clinical isolates of Acinetobacter baumannii in Tehran. Jundishapur J Microbiol 2014;7(1):e8606. DOI: 10.5812/jjm.8606.[pubmed]
40. Rong D, Chun G, Dan H, Ting-ting X, Yan Q. The correlation study on antimicrobial resistance and biofilm related genes in the clinical isolates of Acinetobacter baumannii. Chin Crit Care Med 2013;25(8):493-94. DOI: 10.3760/cma. j. issn.2095-4352. 2013. 08.011.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


