Bacterial pathogens causing UTI and their antibiotic sensitivity pattern: a study from a tertiary care hospital from South India
Abstract
Objectives: This study was conducted to find out the prevalence of pathogens causing UTI and their antibiotic sensitivity pattern.
Materials and Methods: A Prospective study was carried out in the department of Microbiology for one year period from January to December 2018collaboratingwith the various clinical departments to determine the spectrum of organisms causing urinary tract infections and to determine their antibiotic susceptibility profile.
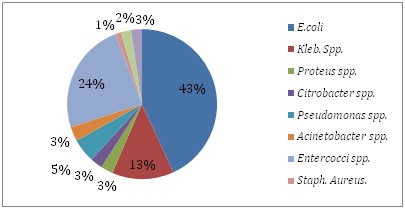
Results: Among the 8303 samples tested significant bacteriuria was observed in 33.14%. The incidence of UTI was more common in females and in the age group of 31-40 years. In this study, 1931 (70.6%) gram negative bacilli and 756 (27.4%) gram positive cocci were isolated, among which E.coli (61.2%) was the commonest followed by Klebsiella (18.90%), Pseudomonas (8.02 %), Acinetobacter (4.4%), Proteus (3.7%) and Citrobacter (3.72%). Among the gram positive organisms Entetrococcus (87.4%) was the highest followed by Coagulase negative staphylococcusaureus (CONS) (7.9%) and Staphlococcus aureus (4.6%). Candida was isolated in 65cases (2.3%). Imipenem (100%) was the most susceptible antibiotic for Enterobacteriaciae followed by levofloxacin (83%) and Amikacin (82%). For the gram positive organisms Vancomycin (100%) and Linezolid (100%) was the most susceptible antibiotic followed by Nitrofurantoin (80%) and Gentamycin (60%). For both the gram positive and the gram negative organisms Nalidicacid, Norfloxacin, Cotrimoxazole and ampicillin were highly resistant and showed less than 30%sensitivity.
Conclusion: Knowledge of the pattern of organisms causing UTI and their sensitivity pattern is important in choosing empirical drugs in the treatment of UTI.
Downloads
References
2. Warren JW. Catheter-associated urinary tract infections. Infect Dis Clin North Am. 1997 Sep;11(3):609-22.[pubmed]
3. Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med. 2012 Mar 15;366(11):1028-37. DOI:10.1056/NEJMcp1104429.[pubmed]
4. Wagenlehner FM, Naber KG. Current challenges in the treatment of complicated urinary tract infections and prostatitis. ClinMicrobiol Infect. 2006 May;12Suppl 3:67-80. DOI:10.1111/j.1469-0691.2006.01398.x
5. Beyene G, Tsegaye W. Bacterial uropathogens in urinary tract infection and antibiotic susceptibility pattern in jimma university specialized hospital, southwest ethiopia. Ethiop J Health Sci. 2011 Jul;21(2):141-6. DOI:10.4314/ejhs.v21i2.69055.[pubmed]
6. Okonko IO, Ijandipe LA, Ilusanya OA, et al. Incidence of urinary tract infection (UTI) among pregnant women in Ibadan, South-Western Nigeria. African Journal of Biotechnology. 2009;8(23):6649–6657.
7. Nerurkar A, Solanky P, Naik SS. Bacterial pathogens in urinary tract infection and antibiotic susceptibility pattern. J Pharm Biomed Sci 2012; 21: 1-3.
8. Moue A, AktaruzzamanSAQM, Ferdous N, Karim R, Khalil MMR, Das AK. Prevalence of urinary tract infection in both outpatient department and in patient department at a medical college setting of Bangladesh. International Journal of Biosciences 2015;7(5):146-152
9. Kripke C. Duration of therapy for women with uncomplicated UTI.AmFam Physician. 2005 Dec 1;72(11):2219.[pubmed]
10. Kahlmeter G; ECO.SENS. An international survey of the antimicrobial susceptibility of pathogens from uncomplicated urinary tract infections: the ECO.SENS Project. J AntimicrobChemother. 2003 Jan;51(1):69-76. DOI:10.1093/jac/dkg028.[pubmed]
11. Eshwarappa M, Dosegowda R, Aprameya IV, et al. Clinico-microbiological profile of urinary tract infection in south India. Indian J Nephrol. 2011 Jan;21(1):30-6. DOI: 10.4103/0971-4065.75226.[pubmed]
12. Akram M, Shahid M, Khan AU. Etiology and antibiotic resistance patterns of community-acquired urinary tract infections in J N M C Hospital Aligarh, India.Ann ClinMicrobiolAntimicrob. 2007 Mar 23;6:4.DOI:10.1186/1476-0711-6-4
13. Kumari SS, Ramya T, Reddy K, Swarnalatha G, Swapna V, Reddy BS, et al. Aetiology and antibiotic resistance pattern of uropathogens in a tertiary care hospital. J Evol Med Dent Sci 2016;5:5534-8.
14. Chongtham U, Yengkokpam C, Lokhendro H. Bacterial uropathogens in urinary tract infection and antibiotic susceptibility pattern of patients attending JNIMS hospital, Imphal. J EvolMed Dental Sci 2013;2:9769-74.
15. Vohra P, Mengi S, Bunger R, Garg S, Pathania D, Singh VA. Bacterial uropathogens in urinary tract infection and their antibiotic susceptibility pattern in a tertiary care hospital. Int J CurrMicrobiol App Sci 2015;4:612-45.
16. V.P.Sarasu, Rani S.R.Bacteriological profile and antibiogram of urinary tract infections at a tertiary care hospital. International Journal of Medical Microbiology and Tropical diseases 2017;3(3):106-112
17. Bahadin J, Teo SS, Mathew S. Aetiology of community-acquired urinary tract infection and antimicrobial susceptibility patterns of uropathogens isolated. Singapore Med J. 2011 Jun;52(6):415-20.[pubmed]
18. Tseng MH, Lo WT, Lin WJ, et al. Changing trend in antimicrobial resistance of pediatric uropathogens in Taiwan. Pediatr Int. 2008 Dec;50(6):797-800. DOI: 10.1111/j.1442-200X.2008.02738.x.[pubmed]
19. Ochei J, Kolhatkar A. Medical Laboratory Science Theory and Practicereprint. 6th edition. New Delhi, India: McGraw-Hill; 2007. Diagnosis of infection by specific anatomic sites/antimicrobial susceptibility tests; pp. 615–643, 788–798.
20. Aiyegoro OA, Igbinosa OO, Ogunmwonyi IN, Odjadjaro E, Igbinosa OE, Okoh AI. Incidence of urinary tract infections (UTI) among children and adolescents in Ile-Ife, Nigeria.African Journal of Microbiological Research. 2007;1:13–19.
21. Orrett FA, Davis GK. A comparison of antimicrobial susceptibility profile of urinary pathogens for the years, 1999 and 2003. West Indian Med J. 2006 Mar;55(2):95-9. DOI:10.1590/s0043-31442006000200006.[pubmed]
22. Desai P, Ukey PM, Chauhan AR, Malik S, Mathur M. Etiology and antimicrobial resistance patterns of uripatyhogens in a hospital from suburb of Mumbai. Int J Biol Med Res 2012; 3: 2007-2012.
23. Ullah F, Malik SA, Ahmed J. Antimicrobial susceptibility pattern and ESBL prevalence in Klebsiella pneumoniae from urinary tract infections in the North-West of Pakistan. African Journal of Microbiology Research. 2009 Nov 30;3(11):676-80.
24. Vromen M, van der Ven AJ, et al. Antimicrobial resistance patterns in urinary isolates from nursing home residents. Fifteen years of data reviewed. J AntimicrobChemother. 1999 Jul;44(1):113-6. DOI:10. 1093/jac/44.1.113
25. Kahlmeter G. Prevalence and antimicrobial susceptibility of pathogens in uncomplicated cystitis in Europe. The ECO. SENS study. INT J Antimicrob Agents. 2003 Oct;22 Suppl 2:49-52. DOI:https://doi.org/10.1016/ S0924-8579(03)00229-2.[pubmed]
26. Sood S, Gupta R. Antibiotic resistance pattern of community acquired uropathogens at a tertiary care hospital in Jaipur, Rajasthan. Indian J Community Med 2012;37:39-44. DOI:https://dx.doi.org/ 10.4103%2F0970-0218.94023
27. Naik TB, Lavanya J, Upadhya A, Mani V. Gram positive uropathogens and their antibiogram: Data analysis at a tertiary care hospital in Karnataka. Indian J Microbiol Res 2018;5(1):71-75. DOI: 10.18231/2394-5478.2018.0014


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


