Histomorphological study of duodenum with special reference to RUT (Rapid Urease Test) negative dyspepsia in a rural care setting
Abstract
Introduction:In our institute duodenal biopsies are taken in patients having either, unexplained anemia, weight loss, recurrent loose stool, abdominal pain, dyspepsia or suspected malabsorption. In the present study we have evaluated histomorphological features of duodenal biopsies in patients presented with specifically Rapid Urease Test (RUT) negative dyspepsia.
Materials and Methods: A retrospective observational study was conducted and data of duodenal biopsies were collected from January 2017 to December 2018. Histopathology slides of duodenal biopsies were reevaluated. We have correlated clinical and endoscopic findings with various histomorphological parameters.
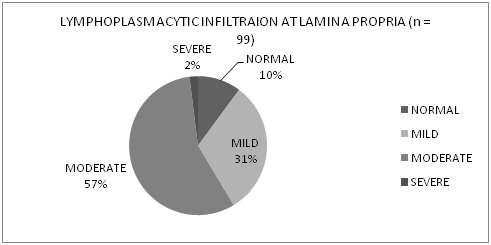
Results: We have included total 99 cases. Demographic profile of our study population shows wide age range (9 years to 74 years) with mean age 39.8 years and Male: Female ratio 1.1:1. Dyspepsia was the common presenting symptoms (64.6% cases) and malabsorption was suspected in 29 cases. 28.3% cases show villous architectural abnormalities which correlate significantly with endoscopic findings of duodenal nodularity. Moderate to severe lamina propria lympho-plasmacytic infiltration seen in 58.56% cases and correlates significantly with dyspeptic symptoms. Duodenal biopsy was diagnostic in 3% cases.
Conclusion: Diagnostic yield of duodenal biopsy is low but informative with proper clinical background.
Downloads
References
2. Talley NJ. American Gastroenterological Association Medical Position Statement: Evaluation of Dyspepsia. Gastroenterology. 2005;129(5):1753-5 DOI: 10.1053/j.gastro.2005.09.019 Available from: https://doi.org /10.1053/j.gastro. 2005.09.019.
3. Riley S, Marsh M. Maldigestion and Malabsorption. Sleisenger and Fordtran’s, Gastrointestinal and Liver Disease, Pathophysiology/Diagnosis/Management. Volume 2. 6th Edition ed: W.B. Saunders company; 1998. p. 1501- 22.
4. Talley NJ, Stanghellini V, Heading RC, et al. Functional gastroduodenal disorders. Gut. 1999 Sep;45 Suppl 2:II37-42. DOI:10.1136/gut.45.2008.ii37.[pubmed]
5. Moayyedi P, Deeks J, Talley NJ, et al. An update of the Cochrane systematic review of Helicobacter pylori eradication therapy in nonulcer dyspepsia: resolving the discrepancy between systematic reviews. Am J Gastroenterol. 2003 Dec;98(12):2621-6. DOI:10.1111/j.1572-0241.2003.08724.x.[pubmed]
6. Kori M, Gladish V, Ziv-Sokolovskaya N, et al. The significance of routine duodenal biopsies in pediatric patients undergoing upper intestinal endoscopy. J Clin Gastroenterol. 2003 Jul;37(1):39-41.[pubmed]
7. Hopper AD, Cross SS, McAlindon ME, et al. Symptomatic giardiasis without diarrhea: further evidence to support the routine duodenal biopsy? Gastrointest Endosc. 2003 Jul;58(1):120-2. DOI:10.1067/mge.2003.199.[pubmed]
8. Stoven SA, Choung RS, Rubio-Tapia A, et al. Analysis of Biopsies From Duodenal Bulbs of All Endoscopy Patients Increases Detection of Abnormalities but has a Minimal Effect on Diagnosis of Celiac Disease. Clin Gastroenterol Hepatol. 2016 Nov;14(11):1582-1588. doi: 10.1016/j.cgh.2016.02.026. Epub 2016 Mar 7.[pubmed]
9. Burger JP, Meijer JW, Wahab PJ. Routine duodenal biopsy to screen for coeliac disease is not effective. The Netherlands journal of medicine. 2013;71(6):308-12 Available from: http://www.njmonline.nl/getpdf.php?id=1331.
10. Basavaraj A, Kulkarni R, Kadam D, Thorat V. Clinicohistopathological correlation and Helicobacter pylori status in patients with functional dyspepsia. Medical Journal of Dr DY Patil University. 2017;10(3):257-62 DOI: 10.4103/0975-2870.206571
11. Stanghellini V, Tosetti C, De Giorgio R, Barbara G, Salvioli B, Corinaldesi R. How should Helicobacter pylori negative patients be managed? Gut. 1999;45 Suppl 1(Suppl 1):I32-5 DOI: 10.1136/gut.45.2008.i32 Available from: https://gut.bmj.com/content/gutjnl/45/suppl_1/I32.full.pdf.
12. Gupta R, Reddy DN, Makharia GK, Sood A, Ramakrishna BS, Yachha SK, et al. Indian task force for celiac disease: current status. World journal of gastroenterology. 2009;15(48):6028-33 DOI: 10.3748/wjg.15.6028
13. Makharia GK, Verma AK, Amarchand R, et al. Prevalence of celiac disease in the northern part of India: a community based study. J Gastroenterol Hepatol. 2011 May;26(5):894-900. doi: 10.1111/j.1440-1746.2010.06606.x.[pubmed]
14. Balasubramanian P, Badhe BA, Ganesh RN, et al. Morphologic Spectrum of Duodenal Biopsies in Malabsorption: A Study from Southern India. J Clin Diagn Res. 2017 Jul;11(7):EC17-EC21. doi: 10.7860/JCDR/2017/23871.10231. Epub 2017 Jul 1.[pubmed]
15. Owen DR, Owen DA. Celiac Disease and Other Causes of Duodenitis. Archives of pathology & laboratory medicine. 2018;142(1):35-43 DOI: 10.5858/arpa.2016-0608-RA.[pubmed]
16. Castro F, Shiroky J, Raju R, Lurix E, Erim T, Johnston Y, et al. Routine Duodenal Biopsies in the Absence of Endoscopic Markers of Celiac Disease Are Not Useful: An Observational Study. ISRN Endoscopy. 2013;2013:5 DOI: 10.5402/2013/623936 Available from: http://dx.doi.org/10.5402/2013/623936.
17. Zukerman GR, Mills BA, Koehler RE, et al. Nodular duodenitis. Pathologic and clinical characteristics in patients with end-stage renal disease. Dig Dis Sci. 1983 Nov;28(11):1018-24.[pubmed]
18. Gonul CD, Bilge C, Gazi KA, Filiz K. Duodenal nodularity in children: a clinical and pathologic study of 17 cases. Indian journal of pathology & microbiology. 2011;54(2):312-7 DOI: 10.4103/0377-4929.81611.[pubmed]
19. Collins JS, Hamilton PW, Watt PC, Sloan JM, Love AH. Quantitative histological study of mucosal inflammatory cell densities in endoscopic duodenal biopsy specimens from dyspeptic patients using computer linked image analysis 1990 [updated AugPMC1378609]. 1990/08/01:[858-61]. Available from: https://gut.bmj.com/content/31/8/858.long.
20. Li XB, Ge ZZ, Chen XY, Liu WZ. Duodenal gastric metaplasia and Helicobacter pylori infection in patients with diffuse nodular duodenitis. Brazilian journal of medical and biological research = Revista brasileira de pesquisas medicas e biologicas. 2007;40(7):897-902 DOI: 10.1590/s0100-879x2006005000117 Available from: http://dx.doi.org/10.1590/S0100-879X2006005000117
21. Fenoglio-Preiser CM, Noffsinger AE, Stemmermann GN, Lantz PE. Gastrointestinal Pathology: An Atlas and Text: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008.
22. Lee YY, Chua AS. Influence of gut microbes on the brain-gut axis (Gut 2011;60:307-317). J Neurogastroenterol Motil. 2011 Oct;17(4):427-9. doi: 10.5056/jnm.2011.17.4.427. Epub 2011 Oct 31.[pubmed]
23. Li X, Chen H, Lu H, et al. The study on the role of inflammatory cells and mediators in post-infectious functional dyspepsia. Scand J Gastroenterol. 2010 May;45(5):573-81. doi: 10.3109/00365521003632576.[pubmed]


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


