Diagnostic utility of inflammatory markers in septic arthritis in pediatric patients in atertiary care hospital in Bangalore
Abstract
Objectives: Septic arthritis is a disease associated with serious morbidity to the patient. The causes of monoarticular arthritis are numerous, with septic arthritis being the most important entity. The diagnosis is rarely established by the history and physical examination, and the clinician is led to rely on ancillary tests.As there are very limited studies relating to the usefulness of CRP, synovial fluid WBCand ESR in diagnosing septic arthritis in the pediatric population, this study was donein pediatric population in a tertiary care hospital in Bangalore.
Materials and Methods: This is a retrospective study done over a period of 24months from January 2017 to December 2018. The study population included all the suspected patients of septic arthritis.Their inflammatory markers like WBC count, ESR and CRP were compared with the culture of the synovial fluid.
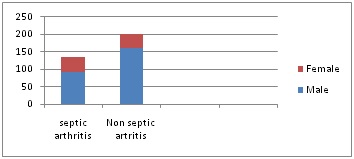
Results: Our records search identified 335 potential cases. 134 cases fulfilled the diagnostic criteria for septic arthritis out of the 335 included in the study. Sensitivity of ESR was: 98% using a cutoff of ≥10 mm/h and 94% using a cutoff of ≥15 mm/h. The sensitivity of CRP was 92% using a cutoff of ≥20 mg/L. synovial fluid sample with WBC of >50 000/μL of which >75% are polymorphonuclear cells is considered to suggest Septic arthritis.
Conclusion: Using our data and comparing it with published data we propose that it is unnecessary to perform further investigation for septic arthritis in patients who have all three of: ESR value <15mm/h, WBC <50,000/μL and CRP value <20mg/l.
Downloads
References
2. Margaretten ME, Kohlwes J, Moore D, et al. Does this adult patient have septic arthritis? JAMA. 2007 Apr 4;297(13):1478-88. DOI:10.1001/jama.297.13.1478.[pubmed]
3. Till SH, Snaith ML. Assessment, investigation, and management of acute monoarthritis. J AccidEmerg Med. 1999 Sep;16(5):355-61.[pubmed]
4. Kaandorp CJ, Van Schaardenburg D, Krijnen P, et al. Risk factors for septic arthritis in patients with joint disease. A prospective study. Arthritis Rheum. 1995 Dec;38(12):1819-25.[pubmed]
5. Saraux A, Taelman H, Blanche P, et al. HIV infection as a risk factor for septic arthritis. Br J Rheumatol. 1997 Mar;36(3):333-7.[pubmed]
6. Kaandorp CJ, Dinant HJ, van de Laar MA, et al. Incidence and sources of native and prosthetic joint infection: a community based prospective survey. Ann Rheum Dis. 1997 Aug;56(8):470-5.[pubmed]
7. Gupta MN, Sturrock RD, Field M. A prospective 2-year study of 75 patients with adult-onset septic arthritis. Rheumatology (Oxford). 2001 Jan;40(1):24-30.[pubmed]
8. Cooper C, Cawley MI. Bacterial arthritis in an English health district: a 10 year review. Ann Rheum Dis. 1986 Jun;45(6):458-63. DOI:10.1136/ard.45.6.458
9. Söderquist B, Jones I, Fredlund H, et al. Bacterial or crystal-associated arthritis? Discriminating ability of serum inflammatory markers. Scand J Infect Dis. 1998;30(6):591-6.[pubmed]
10. Freed JF, Nies KM, Boyer RS, et al. Acute monoarticular arthritis. A diagnostic approach. JAMA. 1980 Jun 13;243(22):2314-6.[pubmed]
11. Weston VC, Jones AC, Bradbury N, et al. Clinical features and outcome of septic arthritis in a single UK Health District 1982-1991. Ann Rheum Dis. 1999 Apr;58(4):214-9.[pubmed]
12. Gupta MN, Sturrock RD, Field M. A prospective 2-year study of 75 patients with adult-onset septic arthritis. Rheumatology (Oxford). 2001 Jan;40(1):24-30. DOI:10.1093/rheumatology/40.1.24.
13. Kroesen S, Widmer AF, Tyndall A, et al. Serious bacterial infections in patients with rheumatoid arthritis under anti-TNF-alpha therapy. Rheumatology (Oxford). 2003 May; 42(5):617-21. DOI:10.1093/ rheumatology/ keg263.[pubmed]
14. Murdoch DM, McDonald JR. Mycobacterium avium-intracellulare cellulitis occurring with septic arthritis after joint injection: a case report. BMC Infect Dis. 2007 Feb 26;7:9. DOI:10.1186/1471-2334-7-9
15. Zalavras CG, Dellamaggiora R, Patzakis MJ, et al. Septic arthritis in patients with human immunodeficiency virus. Clin OrthopRelat Res. 2006 Oct;451:46-9. DOI:10.1097/01.blo.0000229305.97888.17
16. Brigden ML. Clinical utility of the erythrocyte sedimentation rate. Am Fam Physician. 1999 Oct 1;60(5):1443-50.[pubmed]
17. Grzybowski A, Sak JJ. Who discovered the erythrocyte sedimentation rate? J Rheumatol. 2011 Jul;38(7):1521-2; author reply 1523. doi: 10.3899/jrheum.101312.[pubmed]
18. Janson LW, Tischler M. The Big Picture: Medical Biochemistry. New York, NY: McGraw-Hill; 2012.
19. Batlivala SP. Focus on diagnosis: the erythrocyte sedimentation rate and the C-reactive protein test. Pediatr Rev. 2009 Feb;30(2):72-4. doi: 10.1542/pir.30-2-72.[pubmed]
20. Husain TM, Kim DH, C-reactive protein and erythrocyte sedimentation rate in orthopaedics. Univ Pennsylvania Orthop J. 2002;15:13–16.
21.Wilson DA. Immunologic tests. In: Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworth-Heineman; 1990.[pubmed]
22. Isenman DE, Mandle R, Carroll MC. Complement and immunoglobulin biology. In: Hoffman R, Benz EJ, Silberstein LE, Heslop HE, Weitz JI, Anastasi J, eds. Hematology: Basic Principles and Practice. 6th ed. Philadelphia, PA: Elsevier Saunders; 2013:228–246.e4.
23. Kamath S, Lip GY. Fibrinogen: biochemistry, epidemiology and determinants. QJM. 2003 Oct;96(10):711-29. DOI:10.1093/qjmed/hcg129.[pubmed]
24. Nimmerjahn F, Ravetch JV. The anti-inflammatory activity of IgG: the intravenous IgG paradox. J Exp Med. 2007 Jan 22;204(1):11-5. Epub 2007 Jan 16.[pubmed]
25. Salehzadeh F, Noshin A, Jahangiri S. IVIG Effects on Erythrocyte Sedimentation Rate in Children. Int J Pediatr. 2014;2014:981465. doi: 10.1155/2014/981465. Epub 2014 Jan 29.[pubmed]
26. Vermeire S, Van Assche G, Rutgeerts P. C-reactive protein as a marker for inflammatory bowel disease. Inflamm Bowel Dis. 2004;10(5):661–665. doi:10.1097/00054725-200409000-00026
27. Nudelman R, Kagan BM. C-reactive protein in pediatrics. Adv Pediatr. 1983;30:517-47.[pubmed]
28. Jaye DL, Waites KB. Clinical applications of C-reactive protein in pediatrics. Pediatr Infect Dis J. 1997;16(8):735–746; quiz 746–747. doi:10.1097/00006454-199708000-00003
29. Koenig W. High-sensitivity C-reactive protein and atherosclerotic disease: from improved risk prediction to risk-guided therapy. Int J Cardiol. 2013 Oct 15;168(6):5126-34. doi: 10.1016/j.ijcard.2013.07.113. Epub 2013 Aug 24.[pubmed]
30. Silvestre JP, Coelho LM, Póvoa PM. Impact of fulminant hepatic failure in C-reactive protein? J Crit Care. 2010 Dec;25(4):657.e7-12. doi: 10.1016/j.jcrc.2010.02.004. Epub 2010 Apr 8.[pubmed]


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


