Comparative Study of Ziehl-Neelsen Stain versus Fluorescent Microscopy in Diagnosis of Tuberculous Lymphadenitis on FNAC at A Tertiary Care Centre
Abstract
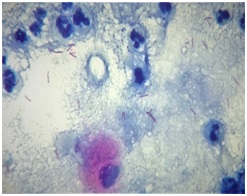
Introduction: Worldwide, TB is one of the top 10 causes of death and the leading cause from a single infectious agent. Lymph nodes tuberculosis is considered the most common form of extrapulmonary tuberculosis and most common cause of lymphadenopathy in developing countries like India.Conventional Ziehl-Neelsen (ZN) method & Fluorescent microscopy (FM) plays an important role for detection of Acid fast bacilli (AFB).
Objectives: This study is an attempt to find out cost effective, rapid and sensitive technique for early diagnosis of tuberculous lymphadenitis. To study incidence, age, sex and site wise distribution of tuberculous lymphadenitis in this area.
Material Methods: The prospective observational study was carried out in the Department of Pathology, S.R.T.R. Govt. Medical College, Ambajogai in year 2017. All 247 aspirated samples from Lymph node swellings were subjected to ZN stain, Fluorescent stain, MGG & PAP stain and 52 cases of tuberculous lymphadenitis were subjected for further analysis,
Results: Out of 247 samples aspirated from lymph node lesions 52 were of tuberculous lymphadenitis (21.05%). For tuberculous lymphadenitis, age ranged from 7 months to 77 years. Female predominance was noted with Female to male ratio 1.17:1. Half of the cases were in the range of 21-40 years of age. Cervical region was the commonest siteinvolved with 51.92%. Of 52 aspirates, smear positivity of AFB on ZN stain method was 78.84%, while positivity of Auramine fluorescent stain method was 90.38%.
Conclusion: In developing countries with high prevalence of tuberculosis, Fine needle aspiration cytology (FNAC) coupled with fluorescent stain & ZN stain could distinctively improve diagnosis of tuberculous lymphadenitis in patients presenting with superficial lymphadenopathy.
Downloads
References
2. Popescu MR, Călin G, Strâmbu I, et al. Lymph node tuberculosis - an attempt of clinico-morphological study and review of the literature. Rom J MorpholEmbryol. 2014;55(2 Suppl):553-67.[pubmed]
3. Krishna M, Kumar A. Tuberculous mycobacteria bacilli fluorescence and compare with Ziehl- Neelsen stain in fine-needle aspiration cytology of tubercular lymphnode. Int J Otorhinolaryngol Head Neck Surg. 2016;2(2):66–9.
4. Thakur B, Mehrotra R, Nigam JS. Correlation of Various Techniques in Diagnosis of Tuberculous Lymphadenitis on Fine Needle Aspiration Cytology Correlation of Various Techniques in Diagnosis of Tuberculous Lymphadenitis on Fine Needle Aspiration Cytology. 2013;(September).
5. Rao VG, Bhat J, Yadav R, Gopalan GP, Nagamiah S, Bhondeley MK, et al. Prevalence of Pulmonary Tuberculosis - A Baseline Survey In Central India. PLoS One [Internet]. 2012 Aug 29;7(8):e43225. Available from: https://doi.org/10.1371/journal.pone.0043225
6. Sandhu GK. Tuberculosis: current situation, challenges and overview of its control programs in India. J Glob Infect Dis. 2011 Apr;3(2):143–50.[pubmed]
7. Singh A, Bhambani P, Nema SK, Singh A, Med JR, Aug S. Diagnostic accuracy of FNAC in diagnosis for causes of lymphadenopathy: a hospital based analysis. Int J Res Med Sci. 2013;1(3):271–7.
8. Gupta R, Dewan D, Suri J. Study of Incidence and Cytomorphological Patterns of Tubercular Lymphadenitis in a Secondary Care Level Hospital of Jammu Region. Indian J Pathol Oncol. 2(3):161–4.
9. Mitra SK, Misra RK, Rai P. Cytomorphological patterns of tubercular lymphadenitis and its comparison with Ziehl-Neelsen staining and culture in eastern up. (Gorakhpur region): Cytological study of 400 cases. J Cytol [Internet]. 2017;34(3):139–43. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28701826
10. Nidhi p, sapna t, shalini m, kumud g. Fnac in tuberculous lymphadenitis: experience from a tertiary level referral centre. Indian j tuberc. 2011;58:102–7.[pubmed]
11. Bezabih M, Mariam DW, Selassie SG. Fine needle aspiration cytology of suspected tuberculous lymphadenitis. Cytopathology. 2002 Oct;13(5):284–90.[pubmed]
12. Bodal VK, Bal MS, Bhagat S, et al. Fluorescent microscopy and Ziehl-Neelsen staining of bronchoalveolar lavage, bronchial washings, bronchoscopic brushing and post bronchoscopic sputum along with cytological examination in cases of suspected tuberculosis. Indian J PatholMicrobiol. 2015 Oct-Dec;58(4):443-7. doi: 10.4103/0377-4929.168849.[pubmed]
13.Githui W, Kitui F, Juma ES, et al. A comparative study on the reliability of the fluorescence microscopy and Ziehl-Neelsen method in the diagnosis of pulmonary tuberculosis. East Afr Med J. 1993 May;70(5):263-6.[pubmed]
14.Ulukanligil M, Aslan G, Tasçi S. A Comparative Study on the Different Staining Methods and Number of Specimens for the Detection of Acid Fast Bacilli. Mem Inst Oswaldo Cruz, Rio Janeiro. 2000;95(6):855–8.[pubmed]
15. Murray SJ, Barrett A, Magee JG, Freeman R. Optimisation of acid fast smears for the direct detection of mycobacteria in clinical samples. J Clin Pathol [Internet]. 2003 Aug;56(8):613–5. Available from: https://www.ncbi.nlm.nih.gov/pubmed/12890813.[pubmed]
16. A. Jain, a. Bhargava, s.k. agarwa. A comparative study of two commonly used staining techniques for acid fast bacilli in clinical specimens. Indian j tuberc. 2002;3(49):161–2.
17. Fazal-i-Wahid, Habib-ur-Rehman Afridi, Muhammad Javaid, Qaisar Khan, Isteraj Khan Shahabi. Tuberculous cervical lymphadenopathy: fnac based study of 100 cases. JMedSci. 2011;19(3):119–21.
18. Bhatta S, Singh S, Chalise SR. Cytopathological patterns of tuberculous lymphadenitis : an analysis of 126 cases in a tertiary care hospital. Int J Res Med Sci. 2018;6(6):1898–901.
19. Ruchira Wadhwa, Purvi Patel, Hansa Goswami, Shveta. ROLE OF FNAC IN TB LYMPHADENITIS. Int J Curr Res. 2017;9(8):55778–81.
20. Goyal R, Kumar A. A Comparison of Ziehl-Neelsen Staining and Fluorescent Microscopy for Diagnosis of Pulmonary Tuberculosis. IOSR J Dent Med Sci. 2013;8(5):5–8.
21. Balakrishna J, Shahapur PR, Chakradhar P, S HS. Comparative Study of Different Staining Techniques - Ziehlneelsen Stain , Gabbet ’ s Stain , Fluorochrome Stain for Detecting of Mycobacterium Tuberculosis in the Sputum . J Pharm Sci Res. 2013;5(4):89–92.
22. Madhusudhan NS, Amirthalingeswaran G. Comparison of ZN Stain ( RNTCP ) Versus Fluorescent Microscopy and Modification of Cold Stain to Detect Acid Fast Bacilli from Sputum Sample. Int J Contemp Med Res. 2016;3(4):968–71.
23. Richards OW, Kline EK, Leach RE. Demonstration of tubercle bacilli by fluorescence microscopy. Vol. 44, Am Rev Tuberc. 2019. 255-266 p.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


