Celiac disease and its histopathology
Abstract
Introduction: Celiac disease, also known as celiac sprue, non-tropical sprue, gluten-induced enteropathy, or gluten-sensitive enteropathy (GSE), is a chronic immune-mediated disorder of the small intestine characterized by malabsorption after ingestion of wheat gluten or related proteins in rye (secalins) and barley (hordeins) in individuals with a certain genetic background.
Materials and Method: The study was conducted in Mahatma Gandhi Medical College and hospital, Jaipur. 53 Duodenal biopsies were taken who have symptoms of diarrhea, iron deficiency anemia, amenorrhea, recurrent mouth ulceration. All biopsies taken from duodenal sitewere brought in 10% buffered formalin. After overnight fixation in formalin, the tissues were processed in automated tissue processor for dehydration, clearing, and paraffin embedding. Sections were cut in rotary microtome 4 micrometer thickness. The section was stained for Hematoxylin and Eosin stain.
Results: The present study included 53 Duodenal biopsies. Out of 53 duodenal biopsies, 12 biopsies have shown presence of Celiac disease. Rest 41 biopsies have shown chronic duodenitis.
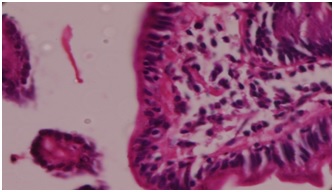
Conclusion: Celiac disease is a common autoimmune condition with mainly intestinal, but also extra-intestinal manifestations. The histologic hallmark of GlutenSensitive Enteropathy is both increased inflammation and architectural derangement in the small intestinal villi.The small intestinal mucosa of untreated persons with celiac disease usually display villous atrophy (Marsh III), or, less commonly, isolated crypt hyperplasia (Marsh II), together with intraepithelial lymphocytic proliferation.
Downloads
References
2. Vincenzo Villanacci ET AL, Coeliac disease: The histology report, Digestive and Liver Disease 43S (2011) S385–S395.[pubmed]
3. Brown IS, Smith J, Rosty C. et al. Gastrointestinal pathology in celiac disease: a case series of 150 consecutive newly diagnosed patients. Am J Clin Pathol. 2012 Jul;138(1):42-9. doi: 10.1309/AJCPE89ZPVJTSPWL.[pubmed]
4. Scanlon SA, et al.Update on celiac disease – etiology, differential diagnosis, drug targets, and management advances. Clin andExp Gastroenterol. 2011;4:297-311. doi: 10.2147/CEG.S8315. Epub 2011 Dec 19.[pubmed]
5. Ludvigsson JF, Leffler DA, Bai JC, et al. The Oslo definitions for coeliac disease and related terms. Gut. 2013 Jan;62(1):43-52. doi: 10.1136/gutjnl-2011-301346. Epub 2012 Feb 16.[pubmed]
6. Vincenzo Villanacci,Coeliac Disease Histopathology, medicel.Unina.it
7. Bao F, Green PH, Bhagat G. An update on celiac disease histopathology and the road ahead. Arch Pathol Lab Med. 2012 Jul;136(7):735-45. doi: 10.5858/arpa.2011-0572-RA.[pubmed]
8. Pudasaini, S. Celiac disease and its histopathology. Journal of Pathology of Nepal, 2017;7(1): 1118-1123.
9. Schuppan D, Zimmer KP. The diagnosis and treatment of celiac disease. DtschArztebl Int. 2013 Dec 6;110(49):835-46. doi: 10.3238/arztebl.2013.0835.[pubmed]
10. Green PH, Cellier C. Celiac disease. N Engl J Med. 2007 Oct 25;357(17):1731-43.[pubmed]
11. Rashtak S, Murray JA. Celiac disease in the elderly. Gastroenterol Clin North Am. 2009 Sep;38(3):433-46. doi: 10.1016/j.gtc.2009.06.005.[pubmed]
12. Ian S. Brown, Update No.7 – 2016 Histopathology of coeliac disease, envoi.come.au
13. Brown I, Mino-Kenudson M, Deshpande V, et al. Intraepithelial lymphocytosis in architecturally preserved proximal small intestinal mucosa: an increasing diagnostic problem with a wide differential diagnosis. Arch Pathol Lab Med. 2006 Jul;130(7):1020-5.[pubmed]
14. MariánŠvajdler ET Al Diagnosing Celiac Disease: Role of the Pathologists International Journal of Celiac Disease, 2014, Vol. 2, No. 2, 70-75
15. de Mascarel A, Belleannée G, Stanislas S, et al. Mucosal intraepithelial T-lymphocytes in refractory celiac disease: a neoplastic population with a variable CD8 phenotype. Am J Surg Pathol. 2008 May;32(5):744-51. doi: 10.1097/PAS.0b013e318159b478.[pubmed]
16. Du MQ, Isaacson PG. First steps in unraveling the genotype of enteropathy-type T-cell lymphoma. Am J Pathol. 2002 Nov;161(5):1527-9. DOI:10.1016/S0002-9440(10)64429-X.[pubmed]
17. Dickson BC, Streutker CJ, Chetty R. Coeliac disease: an update for pathologists. J Clin Pathol. 2006 Oct;59(10):1008-16. DOI:10.1136/jcp.2005.035345.[pubmed]
18. Serra S, Jani PA. An approach to duodenal biopsies. J Clin Pathol. 2006 Nov;59(11):1133-50. Epub 2006 May 5.[pubmed]


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


