Klebsiella Pneumoniae, an Important Uropathogen: Prevalence and Antimicrobial Susceptibility Pattern
Abstract
Introduction: Urinary Tract Infections (UTIs) are amongst the 2nd most common infections after respiratory tract infections in community and healthcare settings (Hospital acquired infections). Klebsiella pneumoniae is the 2nd most common uropathogen after Escherichia coli. Klebsiella is known to have several virulence factors and resistant strains are rising which includes Extended-spectrum Beta-lactamase (ESBL) producing and Carbapenem-resistant strains. Aim of the study is to assess the prevalence of Klebsiella pneumoniae as an Uropathogen and their antimicrobial susceptibility pattern at a tertiary care hospital, Valsad.
Material and Methods: Retrospective study is conducted including isolates of Klebsiella pneumoniae from urine samples received in microbiology laboratory at a tertiary care hospital, Valsad, Gujarat, India from January 2018 to December 2018. Processing of samples, isolation and identification of Klebsiella pneumoniae strains with Antimicrobial susceptibility testing were done using standard microbiology techniques.
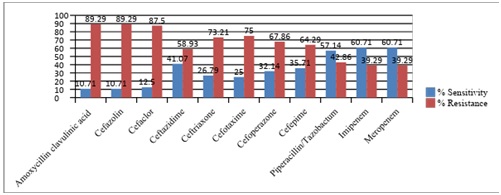
Result: Out of 576 urine samples received in 2018, 209 (36.28%) showed significant growth. Prevalence of Klebsiella pneumoniae as Uropathogen is 9.72% (n=576) and their antimicrobial susceptibility pattern shows higher resistance to β-lactum group (Penicillin, Cephalosporins and Carbapenem). Susceptibility is maximum against Chloramphenicol (87.5%) followed by Nitrofurantoin (64.29%), Amikacin (62.5%), Imipenem (60.71%), Meropenem (60.71%), Levofloxacin (57.14%) and Piperacillin/Tazobactum (57.14%).
Conclusion: Klebsiella pneumoniae remains an important Uropathogen both in community and Hospital acquired infections. Resistance among Klebsiella pneumoniae strains shows upward trends over last few years. Increasing prevalence of ESBL producing and Carbapenem resistant strains creates alarming situation for healthcare system.
Downloads
References
2. Wyres KL, Holt KE. Klebsiella pneumoniae as a key trafficker of drug resistance genes from environmental to clinically important bacteria. CurrOpin Microbiol. 2018 Oct;45:131-139. doi: 10.1016/j.mib.2018.04.004. Epub 2018 May 1.[pubmed]
3. Gatermann SG. Bacterial infections of the urinary tract. In: Borriello P, Murray PR, Funke G, editors. Topley & Wilson’s microbiology & microbial infections, London: Hodder Arnold Publishers 10thed, 2007; vol III:p 671-683.
4. Anila Varghese, Shareen George, Radha kuttyamma Gopalakrishnan, Anna Mathew. Antibiotic susceptibility pattern of Klebsiella pneumoniae isolated from cases of urinary tract infection in a tertiary care setup. J. Evolution Med. Dent. Sci 2016 Apr. 11, 5(29): 1470-1474.
5. Shilpa K, Ruby Thomas and AllavarapuRamyashree. Isolation and Antimicrobial Susceptibility pattern of Klebsiella pneumoniae from sputum samples, International Journal of Biomedical and Advance Research, 2016, 7(02):053-057.
6. SirijanSantajit and NitayaIndrawattana. Mechanisms of Antimicrobial Resistance in ESKAPE Pathogens. BioMed Research International, 2016, Article ID 2475067, http://dx.doi.org/10.1155/2016/2475067.
7. Brews C. Infectious Diseases Society of America. Bad Bugs, No Drugs. As Antibiotic Discovery Stagnates. A Public Health. (2004).
8. Biggest threats and data [Internet]. 2019 [updated 2018 Sep 10; cited 2019 Apr 15]. Available from: https://www.cdc.gov/drugresistance/biggest_threats.html
9. Collee JG, Miles RS, Watt B. Tests for the identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie and McCartney Practical Medical Microbiology. 14th ed. Edinburgh: Churchill Livingstone; 1996. p. 131-150.
10. M100, Performance Standards for Antimicrobial Susceptibility Testing. 28th edition. Pennsylvania, USA: Clinical Laboratory Standard Institute; 2018.
11. Vicky Gandhi, Mehul Patel, Alka Nerurkar. Bacteriological profile and its antibiotic susceptibility in patients with Urinary Tract Infection at Tertiary Care Hospital, Valsad, Gujarat. International Journal of Medical Microbiology and Tropical Diseases, April-June, 2017;3(2):57-60.
12. Harshkumar B. Patel, Sumeeta T. Soni, AroorBhagyalaxmi, Neev M. Patel. Causative agents of urinary tract infections and their antimicrobial susceptibility patterns at a referral center in Western India: An audit to help clinicians prevent antibiotic misuse. J Family Med Prim Care 2019;8:154-9.
13. PareveeDalal, JayshriPethani, HetalSida, Hiral Shah. Microbiological profile of urinary tract infection in a tertiary care hospital, Journal of Research in Medical and Dental Science. Jul-Sep 2016:4(3):204-209.
14. Disha Sharma, Yagnesh Pandya, Suman Singh. Identification, Antimicrobial Resistance Patterns and Factors Associated With Urinary Tract Infections In A Tertiary Care Teaching Hospital of Rural Gujarat-India. Natl J Integr Res Med 2017; 8(5):13-18.
15. Nilofar R. Sodagar, Dr. Sunil S. Trivedi. Microbiological profile and antibiotic susceptibility pattern of Uropathogens in Anand district of Gujarat, India. Journal of Biomedical and Pharmaceutical Research. Jul-Aug 2015;4(4): 51-59.
16. Biswas NK, Patel PH, Ahir HR, Kothadiya PH, Nerurkar AB. Bacteriological Profile Of Urinary Tract Infection And Its Antibiotic Susceptibility At Tertiary Care Hospital, Valsad, Gujarat, India. Journal of Pharmaceutical and Biomedical Science.2014;04(09):751-754.
17. Shankar Shrinivasan, Jovita Saldanha, Suhas Abhyankar, Nikunj Modi, Aakanksha Patil, Arvind M Vartak. Antibiotic Susceptibility pattern of Klebsiella species in burn wounds at Bai Jerbai Wadia hospital for children, Mumbai, India-a 21 year study. Int J Burn Trauma 2017;7(5):64-71.
18. Ritu Bhatnagar, PayalSoni, Sanjeev Kumar, S.K. Mehra, Aruna Solanki, Jyoti Tomar. Study of Nitrofurantoin susceptibility among uropathogenic bacterial isolates at a tertiary care hospital, Udaipur, Rajasthan. World Journal of Pharmaceutical Research. 2015; 4(5): 2124-2132.
19. Sojib Bin Zaman , Muhammed Awlad Hussain , Rachel Nye , Varshil Mehta , KaziTaibMamun , Naznin Hossain. A Review on Antibiotic Resistance: Alarm Bells are Ringing. Cureus 9(6): e1403. DOI 10.7759/cureus.1403.
20. Woldu MA. Klebsiella pneumoniae and Its Growing Concern in Healthcare Settings. Clin Exp Pharmacol. 2016;6: 199. doi:10.4172/2161-1459.1000199.
21. Francis S. Codjoe, Eric S. Donkor. Carbapenem Resistance: A Review. Med Sci (Basel). 2018 Mar; 6(1): 1. doi: 10.3390/medsci6010001.
22. Karen Bush, George A. Jacoby. Updated Functional Classification of β-Lactamases. Antimicrobial agents and chemotherapy. Mar. 2010; 54(3): p. 969–976


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


