Study of the virulence factors and antimicrobial susceptibility profile of staphylococcus aureus isolated from clinical samples at tertiary care centre
Abstract
Introduction: Staphylococcus aureusis an important cause of healthcare-associated infections. The increasing resistance of this pathogen to various antibiotics complicates treatment. Present study was conducted to isolate staphylococcus aureus from various clinical samples, to study the few virulence factors, antibiogram and to detect methicillin resistance among them.
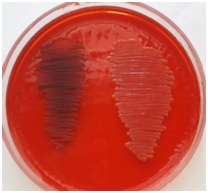
Materials and Methods: Present study was done over a period of six months. The study was conducted on 100 staphylococcus aureus isolated from various clinical samples. The organisms were identified as per standard conventional methods. The antibiotic sensitivity testing of the isolates was done by Kirby Bauer’s Disk Diffusion method according to CLSI guidelines. These strains were screened for DNase production, beta hemolytic property and slime production.
Results: Among 100 clinical isolates of staphylococcus aureus 82% of them showed beta hemolysis, 79% produces DNase, 72% produces slime. The proportion of MRSA amongst S. aureus isolates was found to be 53%. MSSA were 100% sensitive to vancomycin and linezolid85.10 % to Doxycycline, 82.98% to clindamycin, 72.34% to chloramphenicol, 68.09% Co- trimoxozole, 65.95% to erythromycin, 61.70% gentamicin, 51.06 % to Ciprofloxacin, 12.77% topenicillin. MRSA were 100% sensitive to vancomycin and linezolid, 71.69% Doxycycline, 64.15% to Chloramphenicol, 60.37% to Clindamycin, 43.39% to Ciprofloxacin, 39.62% Gentamicin, 37.74% Co- trimoxozole, 35.84% to Erythromycin and all the isolates were resistant to penicillin.
Conclusion: Understanding of virulence mechanisms and antibiotic susceptibility pattern of Staphylococcus aureus is important for effective management of infections.
Downloads
References
2. Perumal N, Dass BS, Mani S, et al. Prevalence of bi-component pore-forming toxin genotypes of Staphylococcus aureus causing skin and soft tissue infections. Indian J Med Microbiol. 2017 Jan-Mar; 35(1):146-147. doi: 10.4103/ijmm.IJMM_16_424.
3. Gitau et al. Antimicrobial susceptibility pattern of Staphylococcus aureus isolates from clinical specimens at Kenyatta National Hospital. BMC Res Notes (2018) 11:226. https://doi.org/10.1186/s13104-018-3337-2.
4. Deotale V, Mendiratta DK, Raut U, et al. Inducible clindamycin resistance in Staphylococcus aureus isolated from clinical samples. Indian J Med Microbiol. 2010 Apr-Jun;28(2):124-6. doi: 10.4103/0255-0857.62488.[pubmed]
5. Alice P. Selvabai et al. Characterization of Methicillin Resistant Staphylococcus aureus based on its virulence factors and antimicrobial susceptibility profile. Indian J Microbiol Res 2017;4(1):74-78.
6. Alli OA, Ogbolu DO, Shittu AO, et al. Association of virulence genes with mecA gene in Staphylococcus aureus isolates from Tertiary Hospitals in Nigeria. Indian J Pathol Microbiol. 2015 Oct-Dec; 58 (4):464-71. doi: 10.4103/0377-4929.168875.[pubmed]
7. Justyna Bien et al. Characterization of Virulence Factors of Staphylococcus aureus: Novel Function of Known Virulence Factors That Are Implicated in Activation of Airway Epithelial Proinflammatory Response. Journal of Pathogens .Volume 2011, Article ID 601905, 13 pages doi:10.4061/2011/601905.
8. Ebrahimi A, Ghasemi M, Ghasemi B. Some Virulence Factors of Staphylococci Isolated From Wound and Skin Infections in Shahrekord, IR Iran. Jundishapur J Microbiol. 2014 Apr;7(4):e9225. doi: 10.5812/jjm.9225. Epub 2014 Apr 1.[pubmed]
9. Collee JG, Marr W. Culture of bacteria. Mackie and McCartney Practical medical microbiology. 14th edn. Edinburg: Churchill Livingstone.1996: 95- 260.
10. Tukyilmaz, et al. Determination of some Virulence Factors in Staphylococcus Spp. Isolated from Various Clinical Samples. Turk J Vet Anim Sci 30 (2006). 127-132.
11. Adrianna Podbielska et al. Slime Production by Staphylococcus aureus and Staphylococcus epidermidis Strains Isolated from Patients with Diabetic Foot Ulcers. Arch. Immunol. Ther. Exp. (2010) 58:321–324. DOI: 10.1007/s00005-010-0079-9 · Source: PubMed.
12. CLSI. Performance Standards for Antimicrobial Susceptibility Testing; 28th ed. Informational Supplement. CLSI document M100-S25. Wayne, PA: Clinical and Laboratory Standards Institute; 2018.
13. Rajaduraipandi K, Mani KR, Panneerselvam K, et al. Prevalence and antimicrobial susceptibility pattern of methicillin resistant Staphylococcus aureus: a multicentre study. Indian J Med Microbiol. 2006 Jan;24(1):34-8.[pubmed]
14. Kale P, Dhawan B. The changing face of community-acquired methicillin-resistant Staphylococcus aureus. Indian J Med Microbiol. 2016 Jul-Sep;34(3):275-85. doi: 10.4103/0255-0857.188313.[pubmed]
15. Kateete et al. Identification of Staphylococcus aureus: DNase and Mannitol salt agar improve the efficiency of the tube coagulase test. Annals of Clinical Microbiology and Antimicrobials 2010, 9:23.http://www.ann-clinmicrob.com/content/9/1/23.
16. Arslan S, Ozkardes F. Slime production and antibiotic susceptibility in staphylococci isolated from clinical samples. Mem Inst Oswaldo Cruz. 2007 Feb;102(1):29-33.[pubmed]
17. Kitara LD, Anywar AD, Acullu D, et al. Antibiotic susceptibility of Staphylococcus aureus in suppurative lesions in Lacor Hospital, Uganda. Afr Health Sci. 2011 Aug;11 Suppl 1:S34-9.[pubmed]
18. Alain C. Juayang. Antibiotic Resistance Profiling of Staphylococcus aureus Isolated from Clinical Specimens in a Tertiary Hospital from 2010 to 2012. Interdisciplinary Perspectives on Infectious Diseases. Volume 2014, Article ID 898457, 4 pageshttp://dx.doi.org/10.1155/2014/898457.
19. Udo EE, Boswihi SS. Antibiotic Resistance Trends in Methicillin-Resistant Staphylococcus aureus Isolated in Kuwait Hospitals: 2011-2015. Med Princ Pract. 2017;26 (5):485-490. doi: 10.1159/000481944. Epub 2017 Oct 4.[pubmed]


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


