Prevalence of non-albicans Candida species versus Candida albicans in critical care patients of a tertiary care hospital
Abstract
Introduction: Candida species are the most common cause of opportunistic fungal infections. Although C.albicans is most common cause of candidiasis, a shift towards non-albicans Candida species is evident in recent years. The transition of Candida spp. from commensal to a potent pathogen is facilitated by a number of virulence factors viz. adherence to host tissues and medical devices, biofilm formation, and secretion of extracellular hydrolytic enzymes.
Objective: To study the prevalence of C.albicans & Non-albicans isolates in critical care settings and determine their virulence factors and antifungal susceptibility profile.
Material & Methods: The present study was carried out in the Department of Microbiology, SGRIMSAR, Amritsar during the period of July 2014 to June 2016. Candida strains isolated from various clinical samples received from different ICUs of the hospital were included in the study. The isolates were identified upto species level by both conventional and automated methods (vitek 2 compact system) as per CLSI guidelines. Relevant history of all the patients was taken. They were also screened for the production of virulence factors such as biofilm formation, haemolytic activity, and production of extracellular hydrolytic enzymes i.e. coagulase.
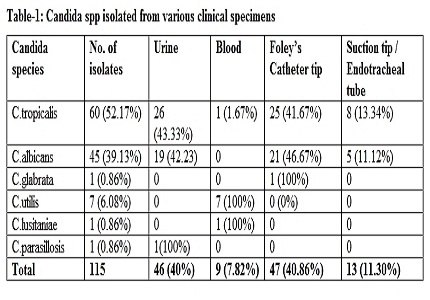
Results: Out of the 115 isolates obtained from various ICUs, most common isolate was C. tropicalis 60/115(52.17%) followed by C. albicans 45/115(39.13%), C.utilis 7/115(6.25%). Isolates of C. lusitaniae, C. parasillosis & C. glabrata were 1/115 (0.86%) each. Among these 95/115(82.6%), 75/115(65.2%), and 83/115(72.17%) isolates showed biofilm formation, coagulase production and haemolytic properties respectively.
Conclusions: Our study showed a shift among Candida species from albicans (39.13%) to non-albicans (60.86%), thus stressing their presence as major fungal pathogens in critical care settings.
Downloads
References
2. Deorukhkar SC, Saini S and Mathew S. Non-albicans Candida Infection: An Emerging Threat.Interdisciplinary Perspectives on Infectious Diseases.2014;1-7.
3. Paul N, Mathai E, Abraham OC, Mathai D. Emerging microbiological trends in Candiduria. Clin Infect Dis. 2004 Dec 1;39(11):1743-4. [PubMed]
4. Giri S, Kindo AJ. A review of Candida species causing blood stream infection. Indian J Med Microbiol. 2012 Jul-Sep;30(3):270-8. doi: 10.4103/0255-0857.99484. [PubMed]
5. Pahwa N, Kumar R, Nirkhiwale S1, Bandi A. Species distribution and drug susceptibility of candida in clinical isolates from a tertiary care centre at Indore. Indian J Med Microbiol. 2014 Jan-Mar;32(1):44-8. doi: 10.4103/0255-0857.124300.
6. Deorukhkar SC, Saini S, Mathew S. Virulence Factors Contributing to Pathogenicity of Candida tropicalis and Its Antifungal Susceptibility Profile. Int J Microbiol. 2014;14:1–6.
7. Kumari V, Banerjee T, Kumar P et al. Emergence of non-albicans Candida among candidalvulvovaginitis cases and study of their potential virulence factors, from a tertiary care center, North India..IJPM 2013;56:144–7.
8. de Oliveira RD, Maffei CM, Martinez R. [Nosocomial urinary tract infections by Candida species]. Rev Assoc Med Bras (1992). 2001 Jul-Sep;47(3):231-5. [PubMed]
9. Oberoi J K, Wattal C, Goel N, Raveendran R, Datta S & Prasad K.. Non-albicans Candida species in blood stream infections in a tertiary care hospital at New Delhi, India. Indian J Med Res 2012; 136: 997-1003.
10. Jain M, Dogra V, Mishra B, Thakur A, Loomba PS, Bhargava A. Candiduria in catheterized intensive care unit patients: emerging microbiological trends. Indian J Pathol Microbiol. 2011 Jul-Sep;54(3):552-5. doi: 10.4103/0377-4929.85091.
11. Bougnoux ME, Gueho E, Potocka AC. Resolutive Candida utilis fungemia in a nonneutropenic patient. J Clin Microbiol. 1993 Jun;31(6):1644-5. [PubMed]
12. Lukić-Grlić A, Mlinarić-Missoni E, Skarić I, Vazić-Babić V, Svetec IK. Candida utilis candidaemia in neonatal patients. J Med Microbiol. 2011 Jun;60(Pt 6):838-41. doi: 10.1099/jmm.0.023408-0. Epub 2011 Feb 24. [PubMed]
13. Shivadasan J, Raksha, Prashanth S Urs. Candida utilis causing neonatal Candidemia – A case report and literature review. Apollo Medicine. 2016;13 ( 1): 55–8.
14. Rodrigues AG, Pina-Vaz C, Costa-de-Oliveira S, Tavares C. Expression of plasma coagulase among pathogenic Candida species. J Clin Microbiol. 2003 Dec;41(12):5792-3. [PubMed]
15. Yigit N, Aktas AE, Ayyildiz A. Detection of coagulase activity in pathogenic Candida species. J Int Med Res. 2008 Nov-Dec;36(6):1378-82. [PubMed]
16. Bizerra FC, Nakamura CV, de Poersch C, Estivalet Svidzinski TI, Borsato Quesada RM, Goldenberg S, Krieger MA, Yamada-Ogatta SF. Characteristics of biofilm formation by Candida tropicalis and antifungal resistance. FEMS Yeast Res. 2008 May;8(3):442-50. doi: 10.1111/j.1567-1364.2007.00347.x. Epub 2008 Jan 29.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


