Seroprevalence of HBV, HCV and HIV infections in blood donors in voluntary and replacement donors in a tertiary care hospital in Western Uttar Pradesh, India
Abstract
Background: The World Health Organization recommends universal and quality-controlled screening of blood donations for the major transfusion-transmissible infections (TTIs): human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV) and syphilis. The magnitude of transfusion-transmitted infections (TTI) varies from country to country depending on TTI’s load in that particular population. The present study was undertaken to determine the relative proportion of voluntary donors (VDs) and replacement donors (RDs) and also, to estimate and compare the seroprevalence and changing trends of TTIs amongst VDs and RDs in a tertiary care medical hospital in north India.
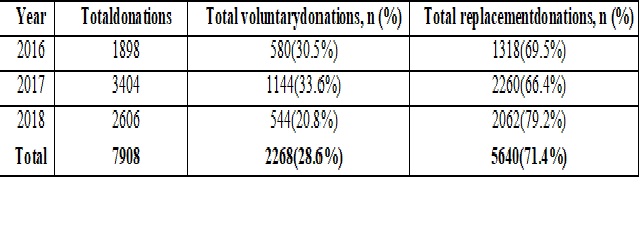
Methods: This retrospective study was based on the records of all voluntary and replacement donations whichwere collected from January 2016to August 2018 in atertiary care medical college and hospital in Bareilly, Uttar Pradesh, India.
Results:Of the total 7908 donations, 2268 (28.6%) were voluntary and 5640 (71.4%) werereplacement donation. The overall seroprevalence of TTI was 158 (1.9%) out of total 7908 donations, with prevalence ofhepatitis B virus (HBV), hepatitis C virus (HCV) and human immunodeficiency virus (HIV), were 1.0, 0.8 and 0.1 percent, respectively. Furthermore, the TTIs were more frequently encountered in RDs in comparison to VDs.
Conclusions: The potential risk of TTIS can be curtailed to a large extent by increasing in public awareness regarding voluntary blood donation, donor screening using stringent criteria, counselling anduse of highly sensitive and specific tests.
Downloads
References
2. ManzoorI,HashmNI,DaudS,AjmalS,FatimaH,RasheedZ,etal.Sero- prevalenceoftransfusiontransmissibleinfections(TTIS)inblooddonors.Biomedica.2009;25(10):154–8.
3. Wasfi OA, Sadek NA. Prevalence of hepatitis B surface antigen and hepatitis C virus antibodies among blood donors in Alexandria, Egypt. East Mediterr Health J. 2011;17(3):238-42.[pubmed]
4. SaghirSAM,HassanFMA,AlsalahiOSA,AlhariryAEAA,BaqirHS.FrequenciesofHBV,HCV,HIV,andsyphilismarkersamongblooddonors:ahospital-basedstudyinHodeidah,Yemen.Trop J Pharm Res.2012;11(1):132–6.
5.SinghR,VohraP,SinglaP,ChaudharyU.Seroprevalenceoftransfusiontransmissibleinfectionsamonghealthyblooddonorsatgeneralhospital,Sonepath,NorthIndia.J Evol Med Dent Sci.2013;2(26):4816–20.
6. Chaudhary IA, Samiullah, Khan SS, Masood R, Sardar MA, Mallhi AA. Seroprevalence of HBV and C among health donors at Fauji Foundation Hospital, Rawalpindi. Pak Med J 2007;23: 64-7.
7.Mollah AH, Nahar N, Siddique MA, et al. Common transfusion-transmitted infectious agents among thalassaemic children in Bangladesh. J Health PopulNutr. 2003 Mar;21(1):67-71.[pubmed]
8. Blood safety, a strategy for the African region. AFR/RC51/R2. Brazzaville, WHO Regional Office for Africa, 2001.
9. Tapko J.B., Mainuka P., Diarra-Nama A.J. Status of blood safety in the WHO African Region, report of the 2006 survey. Brazzaville, WHO Regional Office for Africa, 2009.[pubmed]
10. Tagny C.T., Owusu-Ofori S., Mbanya D., Deneys V. The blood donor in sub-Saharan Africa: a review.Transfus Med., 2010;20(1):1–10.[pubmed]
11. Ward JW, Deppe DA, Samson S, Perkins H, Holland P, Fernando L, et al. Risk of human immunodeficiency virus infection from blood donors who later developed the acquired immunodeficiency syndrome. Ann Intern Med 1987;106:61-28.
12. Arora D, Arora B, Khetarpal A. Seroprevalence of HIV, HBV, HCV and syphilis in blood donors in Southern Haryana. Indian J PatholMicrobiol. 2010 Apr-Jun;53(2):308-9. doi: 10.4103/0377-4929.64295.[pubmed]
13. Singh K, Bhat S, Shastry S. Trend in seroprevalence of Hepatitis B virus infection among blood donors of coastal Karnataka, India. J Infect Dev Ctries. 2009;3(5):376-9.[pubmed]
14. Jain A, Rana SS, Chakravarty P, et al. The prevalence of hepatitis C virus antibodies among the voluntary blood donors of New Delhi, India. Eur J Epidemiol. 2003;18(7):695-7.[pubmed]
15. Zaraski JP, Bohn B, Bastie A, Pawlotsky JM, Baud M, Bost B. Characteristics of patients with dual infection by hepatitis B and C viruses. J Hepatol.1998;28:27-33.[pubmed]
16. National Blood Policy 2007, National Aid Control Organization, Ministry of Health & Family Welfare, Government of India. Available from: www.naco.nic. in. Accessed 12-03-2013
17. Country Scenario – an update; National Aids Control Programme India, December 1996
18. Agarwal VK, Sharma VP, Agrawal P, Gupta D. Sero-prevalence of transfusion transmissible infections among blood donors in urban area. Asian J Med Res 2012; 1: 112-4.
19. Gupta N, Kumar V, Kaur A. Seroprevalence of HIV, HBV, HCV and syphilis in voluntary blood donors. Indian J Med Sci. 2004;58(6):255-7.[pubmed]
20. Jasani J, Patel V, Bhuva K, Vachhani A, Patel H, Falleiro JJJ. Seroprevalence of transfusion transmissible infections among blood donors in a tertiary care hospital. Int J Biol Med Res 2012; 3: 1423-5
21. ChattorajA, Behl R, Kataria VK. Infectious Disease Markers in Blood Donors. Med J Armed Forces India. 2008;64(1):33-5. doi: 10.1016/S0377-1237(08)80142-6. Epub 2011 Jul 21.[pubmed]


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


