A study on Vulvovaginal candidiasis among non-pregnant women
Abstract
Introduction: Candida species are opportunistic pathogens which cause a wide variety of infections in humans ranging from trivial intertriginous infection to fatal candidemia. Vulvo vaginal candidiasis (VVC) is an acute inflammatory disease and a frequent reason for gynaecological consultations. The present study aimed at determining prevalence of Candida species from VVC and to speciate isolated Candida with antifungal susceptibility profile among non pregnant women.
Materials and Methods: This was a cross sectional study conducted over a period of six monthsin the department of microbiology and Obstetrics and Gynecology. Swabs collected from patients were subjected to microscopy (Gram s stain) and culture on Sabouraud’s dextrose agar. Species level was identified by using chrome agar. Antifungal susceptibility
testing: Antifungal susceptibility testing was performed by NCCLS M44 -A Disc diffusion method.
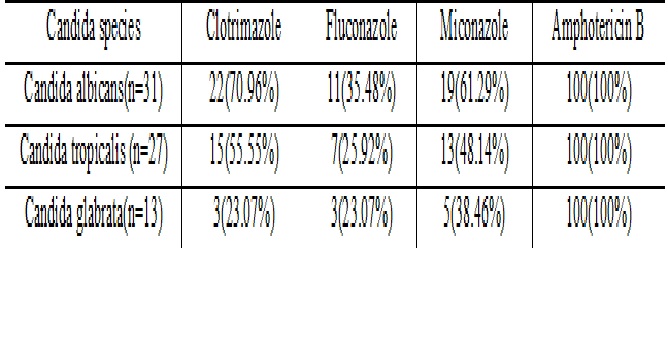
Results: A total of 209 high vaginal swabs were collected from non pregnant women. 71 patients high vaginal swabs yielded growth of Candida species and accounted for 33.97%. Most commonly isolated species were Candida albicans 31 (43.66%) followed by Candida tropicalis 27(38.03%) and Candida glabrata 13(18.31%). All species were found to be susceptible to Amphotericin B. Among commonly used antifungals, clotrimazole was found to be most susceptible. But, C.glabrata species was least susceptible to frequently used antifungals.
Conclusion: Candida albicans was the most commonly isolated species.CHROMagar is rapid, technically simple and cost effective compared to time consuming technically demanding expensive conventional methods. Performing antifungal susceptibility is useful in choosing appropriate antifungal in treating vulvo vaginal candidiasis.
Downloads
References
2. Borges S, Silva J, Teixeira P. The role of lactobacilli and probiotics in maintaining vaginal health. Arch Gynecol Obstet. 2014 Mar;289(3):479-89. doi: 10.1007/s00404-013-3064-9. Epub 2013 Oct 30. [pubmed]
3. Sobel JD, Faro S, Force RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol. 1998 Feb;178(2):203-11.[pubmed]
4. Ahmad A, Khan AU. Prevalence of Candida species and potential risk factors for vulvovaginal candidiasis in Aligarh, India. Eur J ObstetGynecolReprod Biol. 2009 May;144(1):68-71. doi: 10.1016/j.ejogrb.2008.12.020. Epub 2009 Mar 3.[pubmed]
5. Jindal N, Gill P, Aggarwal A. An epidemiological study of vulvovaginal candidiasis in women of childbearing age. Indian J Med Microbiol. 2007 Apr;25(2):175-6.[pubmed]
6. Flowers SA, Colón B, Whaley SG, et al. Contribution of clinically derived mutations in ERG11 to azole resistance in Candida albicans. Antimicrob Agents Chemother. 2015 Jan;59(1):450-60. doi: 10.1128/AAC.03470-14. Epub 2014 Nov 10.[pubmed]
7. Wortman JR, Gilsenan JM, Joardar V, The 2008 update of the Aspergillus nidulans genome annotation: a community effort. Fungal Genet Biol. 2009 Mar;46 Suppl 1:S2-13. doi: 10.1016/j.fgb.2008.12.003. Epub 2008 Dec 25.[pubmed]
8. Wayne, P.A.: Method for Antifungal Disk Diffusion Susceptibility Testing of Yeasts, NCCLS document M44 -A (2004).
9. Enweani IB, Gugnani HC, Okobia R, Ojo SB. Effect of contraceptives on the prevalence of vaginal colonization with Candida species in Edo State, Nigeria. Rev IberoamMicol. 2001 Dec;18(4):171-3.[pubmed]
10. Eckert LO, Hawes SE, Stevens CE, et al. Vulvovaginal candidiasis: clinical manifestations, risk factors, management algorithm. Obstet Gynecol. 1998 Nov;92(5):757-65.[pubmed]
11. Mahadani JW, Dekate RR, Shrikhande AV.Cytodiagnosis of discharge per vaginum. Indian J Pathol Microbiol. 1998 Oct;41(4):403-11.[pubmed]
12. Nandan D, Gupta YP, Krishnan V, et al. Reproductive tract infection in women of reproductive age group in Sitapur/Shahjahanpur District of Uttar Pradesh. Indian J Public Health. 2001 Jan-Mar;45(1):8-13.[pubmed]
13. Aring BJ, Mankodi PJ, Jasani JH. Incidence of vaginal candidiasis in leucorrhoea in women attending in OPD of gynecology and obstetrics department. Int J Biomed Adv Res. 2012;3(12):867–869.
14. Fernández Limia O, Lantero MI, Betancourt A, et al. Prevalence of Candida albicans and Trichomonas vaginalis in pregnant women in Havana City by an immunologic latex agglutination test. MedGenMed. 2004 Oct 15;6(4):50.[pubmed]
15. Alo MN, Anyim C, Onyebuchi AK, Okonkwo EC. Prevalence of asymptomatic co-Infection of candidiasis and vaginal trichomoniasis among pregnant women in Abakaliki, South-Eastern Nigeria. J Nat Sci Res. 2012;2(7):87–91.
16. Okungbowa FI, Isikhuemhen OS, Dede AP. The distribution frequency of Candida species in the genitourinary tract among symptomatic Individuals in Nigerian cities. Rev IberoamMicol. 2003 Jun;20(2):60-3.[pubmed]
17. Habibipour R. Prevalence Rate of Vulvovaginal Candidiasis and Identification ofCandida Species inWomen in Referred to Hamedan Hospitals 2013-2014,West of Iran. Zahedan J Res Med Sci. 2013; 18(3):6250.
18. Corsello S, Spinillo A, Osnengo G, et al. An epidemiological survey of vulvovaginal candidiasis in Italy. Eur J ObstetGynecolReprod Biol. 2003 Sep 10;110(1):66-72.[pubmed]
19. Nazeri M, Mesdaghinia E, Moravej SAR, Atabakhshiyan R, SoleymaniF. Prevalence of vulvovaginal candidiasis and frequency of Candidaspecies in women [in Persian]. J Mazandaran Univ Med Sci.2012;21(86):254–62.
20. Simões JA, Giraldo PC, Faúndes A. Prevalence of cervicovaginal infections during gestation and accuracy of clinical diagnosis. DOI:10.1155/S1064744998000246
21. Bauters TG, Dhont MA, Temmerman MI, Nelis HJ. Prevalence of vulvovaginal candidiasis and susceptibility to fluconazole in women. Am J Obstet Gynecol. 2002 Sep;187(3):569-74.[pubmed]
22.Reed BD. Risk factors for Candida vulvovaginitis. ObstetGynecolSurv. 1992 Aug;47(8):551-60. [pubmed]
23. Mishra M, Agrawal S, Raut S, et al. Profile of yeasts isolated from urinary tracts of catheterized patients. J Clin Diagn Res. 2014 Feb;8(2):44-6. doi: 10.7860/JCDR/2014/6614.4003. Epub 2014 Feb 3.[pubmed]
24. Khan M, Ahmed J, Gul A, Ikram A, Lalani FK. Antifungal susceptibility testing of vulvovaginal Candida species among women attending antenatal clinic in tertiary care hospitals of Peshawa.2018;11:447-56.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


