Seroprevalence and trends of transfusion transmissible infections among voluntary and replacement donors–an institutional retrospective study
Abstract
Introduction:Transfusion transmitted infections are major problem associated with blood transfusion. There are several infectious as well as non-infectious risks associated with transfusion of blood. Aim and
Objective:The present study was carried out to find out the sero-prevalence and changing trends of various TTIs in blood donors.
Material andMethods:A record based study was conducted from January 2008- December 2010. Data were collected from therecords of blood bank which also included data of blood donation camps. Data regarding sex, screening testresults and type of donors were collected from the records.
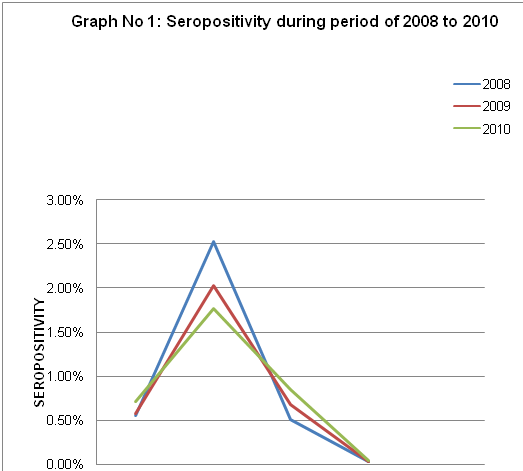
Results:Out of 17640 donors, voluntary donors (78.4%) were more in comparison to replacement donors (21.6%). Out of all TTIs, prevalence of HBV (2.14%) was highest followed by, HCV (0.66%), HIV (0.6%), Malaria (0.14%) and Syphilis (0.05%).TTIs were more prevalent in replacement donors than voluntary donors. The number ofvoluntary donors has fallen from 2008 -2010, but there is male preponderance in both voluntary and replacement donors.
Conclusion:From results it has been concluded that prevalence of transfusion transmitted infection (HIV, HBV, HCV, VDRL, and malaria) was more in replacement donors in comparison to voluntary donors. With the implementation of strict donor selection criteria, use of sensitive screening tests and establishment of strict guidelines for blood transfusion it may be possible to reduce the incidence of transfusion transmitted infection in the Indian scenario.
Downloads
References
2. Suresh B, Sreedhar Babu KV, Arun R, Chandramouli P, Jothibai DS. Reasons for discarding whole blood and its components in a tertiary care teaching hospital blood bank in South India. J Clin Sci Res 2015;4:213-9. DOI: http://dx.doi.org/10.15380/2277-5706.JCSR.14.052.
3.Sunderam S, KarirS,HaiderS,SinghS.B,KiranA.Sero-Prevalence of Transfusion Transmitted Infections among Blood Donors at Blood Bank of Rajendra Institute of Medical Sciences, Ranchi.Healthline Journal 2015;6(1):36-40.
4. Sahil Sehgal, P.S Shaiji, Rupinder Kaur Brar.Seroprevalence and Trends of Transfusion Transmissible Infections in Blood Donors in Andaman and Nicobar Islands- An Institutional Retrospective Study. JCDR 2017;11(4): EC21-EC24.
5. Millennium Development Goals. http://www.who.int/mdg/goals/en/index.html
6. Voluntary Blood Donation Programme—An Operational Guideline, National AIDS Control Organisation, Ministry of Health and Family Welfare Government of India, New Delhi, India,2007.
7. A. Gharehbaghian. An estimate of transfusion-transmitted infection prevalence in general populations. HepatitisMonthly,vol. 11, no. 12, pp. 1002–1003, 2011.
8. Shah N, Shah JM, Jhaveri P, Patel K, Shah CK, Shah NR.Seroprevalence of HBV, HCV, HIV and syphilis among blood donors at a tertiary Care Teaching Hospital in Western India. Gujarat Medical Journal.2013; 68(2): 35-39
9.Patel PA, Patel SP, Oza HV. Seroprevalence of Transfusion Transmitted Infections (TTIs) in blood donors at Western Ahmedabad – a secondary care hospital based study. Int J Biol Med Res. 2012;3:1806-10.
10. Kulkarni N. Analysis of the seroprevalence of HIV, HBsAg, HCV, & Syphilitic infections detected in the pre transfusion blood: A short report. Int J Blood Transfus Immunohematology. 2012;2:1-3..
11. Arora D, Arora B, Khetarpal A. Seroprevalence of HIV, HBV, HCV and syphilis in blood donors in Southern Haryana. doi: 10.4103/0377-4929.64295 . [pubmed]
12. Pallavi P, Ganesh CK, Jayashree K, Manjunath GV. Seroprevalence and trends [7]in transfusion transmitted infections among blood donors in a university hospital blood bank: a 5 year study. Indian J Hematol Blood Transfus. 2011;27:1–6.
13. Singh K, Bhat S, Shastry S. Trend in seroprevalence of Hepatitis B virus infection among blood donors of coastal Karnataka, India. J Infect Dev Ctries. 2009 Jun 1;3(5):376-9. [pubmed]
14. Singh B, Verma M, Kotru M, et al. Prevalence of HIV and VDRL seropositivity in blood donors of Delhi. Indian J Med Res. 2005 Sep;122(3):234-6. [pubmed]
15. Pahuja S, Sharma M, Baitha B, Jain M. Prevalence and trends of markers of hepatitis C virus, hepatitis B virus and human immunodeficiency virus in Delhi blood donors: a hospital based study. Jpn J Infect Dis. 2007 Nov;60(6):389-91.[pubmed]
16. Chandra T, Kumar A, Gupta A. Prevalence of transfusion transmitted infections in blood donors: an Indian experience.doi: 10.1258/td.2008.080330. [pubmed]
17. Sawke N, Sawke G K, Chawla S. Seroprevalence Of Common Transfusion–Transmitted infections among Blood Donors at Bhanpur, Bhopal, M.P. from 2006–2008.Peoples J Of sci.Research 2010;3(1) 5-7.
18. Bhawani Y, Rao PR, Sudhakar V. Seroprevalence of transfusion transmissible infections among blood donors in a tertiary care hospital of Andhra Pradesh from. 2004–2009.Biology and Medicine 2010;2(4): 45-48.
19. Jasani J, Patel V, Bhuva K, Vachhani A, Patel H, Falleiro JJ. Seroprevalence of transfusion transmissible infections among blood donors in a tertiary care hospital. Int J Biol Med Res. 2012; 3(1):1423-1425.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


