A study of bacteriological and antibiotic susceptibility profile of urinary tract infection
Abstract
Introduction: Urinary tract infection (UTI) is one of the most common infection and is associated with significant morbidity in the community. Most of the UTI cases are treated empirically with broad-spectrum antibiotics which invariably results in the development of resistance. Aims and
Objectives: The objective of this study was to determine the antibiotic susceptibility pattern of bacterial isolates causing UTI and to determine Extended spectrum beta Lactamase (ESBL) production in Gram negative isolates.
Materials and Methods: A total of 724 urine samples were studied and bacteria identified by standard microbiological methods. Antibiotic sensitivity pattern was done by Kirby-Bauer disc diffusion method. Detection of ESBL was done as per Clinical and Laboratory Standards Institute (CLSI) guidelines.
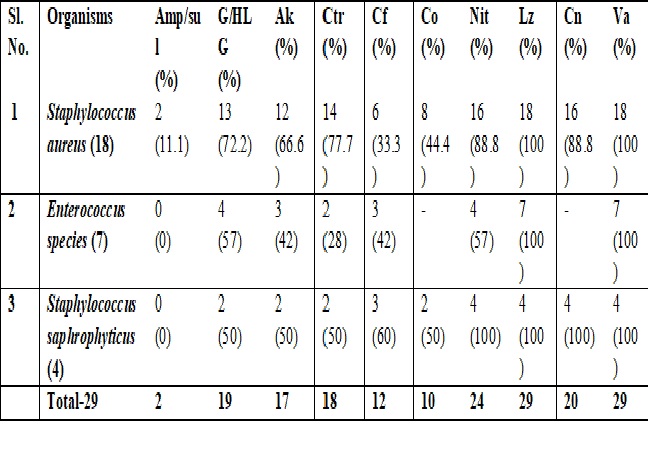
Results: Significant bacteriuria was detected in 238 (32.8%) samples. The most common pathogens isolated were Escherichia coli 148 (58.9%), Klebsiella pneumoniae 57 (22.7%) and Staphylococcus aureus 18 (7.1%) followed by Enterococcus spp 7 (2.7%), Proteus mirabilis 6 (2.4%), Citrobacter koseri 6 (2.4%), Pseudomonas aeruginosa 5(2%) and Staphylococcus saphrophyticus 4 (1.6%). ESBL production was seen in Klebsiella pneumoniae 12 (21%), followed by Escherichia coli 26 (17.5%). Most of the Gram-negative bacteria were susceptible to meropenam, piperacillin-tazobactum and nitrofurantoin.
Conclusion: This study reveals that many bacteria causing UTI are multidrug resistant pathogens. This suggests that regular monitoring and modification of empirical therapy and it’s validation by culture report is required to prevent morbidity associated with this disease.
Downloads
References
2. Kaushik C, Gangadhar NK, Subrahmanya BK, Kotigadde S. Anti-biogram pattern of uro-pathogens isolated from patients in a Tertiary Care Hospital in Karnataka, India. Indian J Microbiol Res 2018;5(1):24-30.
3. Niranjan V, Malini A. Antimicrobial resistance pattern in Escherichia coli causing urinary tract infection among inpatients. Indian J Med Res 2014;139(6):945–8.[pubmed]
4. Renuart AJ, Goldfarb DM, Mokomane M, Tawanana EO, Narasimhamurthy M, Steenhoff AP. (2013). Microbiology of Urinary Tract Infections in Gaborone, Botswana. PLOS ONE. 4;8(3):e57776.[pubmed]
5. Arias CA, Murray BE. Antibiotic-resistant bugs in the 21st century--a clinical super-challenge. N Engl J Med 2009;29(5):439–43.[pubmed]
6. Aruna K, Mobashshera T. Prevalence of extended spectrum beta-lactamase production among uropathogens in south Mumbai and its antibiogram pattern. EXCLI Journal 2012;11(7):363-72.[pubmed]
7. Rupp ME, Fey PD. Extended spectrum β-lactamase (ESBL)- producing enterobacteriaceae: Staphylococcus saphrophyticus. Considerations for diagnosis, prevention and drug treatment. Drugs J 2003;63(4):353–65.
8. Colodner R. Extended-spectrum beta-lactamases: a challenge for clinical microbiologists and infection control specialists. Am J Infect Control 2005;33(2):104–7.[pubmed]
9. Deshmukh DG, Damle AS, Bajaj JK, Bhakre JB, Patwardhan NS. Metallo- ß-lactamase-producing clinical isolates from the patients of a tertiary care hospital. J Lab Physicians 2011;3:93-7.[pubmed]
10. Manjunath GN, Prakash R, Annam V, Shetty K. Changing trends in the spectrum of antimicrobial drug resistance pattern of uropathogens isolated from hospitals and community patients with urinary tract infections in Tumkur and Bangalore. Int J Biol Med Res 2011;2(2):504-7.
11. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; (2017).27th informational supplement, Wayne, PA, USA. 2017;32(3) M100-S27.
12. Magale Hi, Kassim Ia, Odera Sa, Omolo Mj, Jaoko Wg, Jolly Pe. Antibiotic Susceptibility Of Organisms Causing Urinary Tract Infection In Patients Presenting At Kenyatta National Hospital, Nairobi. East Afr Med J 2015;92(7):333–7.[pubmed]
13. Das RN, Chandrashekhar TS, Joshi HS, Gurung M, Shrestha N, Shivananda PG. Frequency and susceptibility profile of pathogens causing urinary tract infections at a tertiary care hospital in western Nepal. Singapore Med J 2006;47(4):281–5.[pubmed]
14. Gonzalez CM, Schaeffer AJ. Treatment of urinary tract infection: what’s old, what’s new, and what works. World J Urol 2001;17(6):372–82.[pubmed]
15. Orrett F A. Urinary tract infections in general practice in a rural community in South Trinidad. Saudi Med Journal 2001;22:537–40.[pubmed]
16. Sood S, Gupta R. Antibiotic resistance pattern of community acquired uropathogens at a tertiary care hospital in Jaipur, Rajasthan. Indian J of Communi Medi 2012;37:39–44.
17. Gupta N, Kundra S, Sharma A, GautamV, Arora DR. Antimicrobial susceptibility of uropathogens in India. J Infect Dis Antimicrob Agents 2007;24:13-8.
18. Prakash D, Saxena RS. Distribution and Antimicrobial Susceptibility Pattern of Bacterial Pathogens Causing Urinary Tract Infection in Urban Community of Meerut City, India. ISRN Microbiology 2013;6:56-78.[pubmed]
19. Poudyal S, Bhatta DR, Shakya G, Upadhyaya B, Dumre SP, Buda G, et al. Extended Spectrum beta-lactamase producing multidrug resistant clinical bacterial isolates at National Public Health Laboratory, Nepal. Nepal Med Coll J 2011;13(1):34–8.
20. Sundaramurthy R, Tiruvanamalai R, Sivaraman ST, Arunagiri R, Charles J. Study on clinico microbiological profile and antibiotic susceptibility pattern of urinary tract pathogens with Special reference to susceptibility of Escherichia coli to fosfomycin. Indian J of Microbiol Res 2018;5(2):258-65
21. Nepal K, Pant ND, Neupane B, Belbase A, Baidhya R, Shrestha RK, et al. Extended spectrum beta‑lactamase and metallo beta‑lactamase production among Escherichia coli and Klebsiella pneumoniae isolated from different clinical samples in a tertiary care hospital in Kathmandu, Nepal . Ann Clin Microbiol Antimicrob 2017;16:62:1-7.[pubmed]
22. Yadav KK, Adhikari N, Khadka R, Pant AD, Shah B. Multidrug resistant Enterobacteriaceae and extended spectrum β-lactamase producing Escherichia coli: a cross-sectional study in National Kidney Center, Nepal. Antimicrob Resist Infect Control 2015;4:42.[pubmed]
23. Pilli R, Kapaganty VC. Study of extended spectrum beta lactamase producing uropathogens and their antibiotic susceptibility pattern. Indian J of Microbiol Res 2018;5(2):280-83.
24. Eshwarappa M, Dosegowda R, Aprameya IV, Khan MW, Kumar PS, Kempegowda P. Clinico-microbiological profile of urinary tract infection in South India. Indian J Nephrol 2011;21(1):30-3.[pubmed]
25. Kader AA, Kumar AK. Prevalence of extended spectrum beta-lactamase among multidrug resistant gram-negative isolates from a general hospital in Saudi Arabia. Saudi Med J 2004;25:570–4.[pubmed]
26. Shashwati N, Kiran T, Dhanvijay AG. Study of extended spectrum β-lactamase producing Enterobaceriaceae and antibiotic co-resistance in a tertiary care teaching hospital. J Nat Sci Biol Med 2014;5:30–5.
27. Naik TB, Lavanya J, Upadhya A, Mani V. Gram positive uropathogens and their antibiogram: Data analysis at a tertiary care hospital in Karnataka. Indian J Microbiol Res 2018;5(1):71-5.
28. Bajpai T, Pandey M, Varma M, Bhatambare GS. Prevalence of extended spectrum beta-lactamase producing uropathogens and their antibiotic resistance profile in patients visiting a tertiary care hospital in central India: Implications on empiric therapy. Indian J Pathol Microbiol 2014;57(3):407-12.[pubmed]


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


