Carrier status of Acinetobacter among healthcare personnel and prevalence of the same in the environment
Abstract
Background: Acinetobacter baumanii is an increasingly troublesome nosocomial pathogen, often with multidrug and multi resistant strains, mainly in intensive care units (ICUs), being responsible for different types of nosocomial infections.
Objectives: The objective was to determine prevalence of carriers of Acinetobacter Spp. and predisposing risk factors among healthcare workers (HCWs) in ICUs and their role as source in nosocomial infection.
Materials and Methods: Specimens from nose, throat, axilla and hands of all HCWs (55 (40 staff nurses, 15 attenders)) from ICUs and 30 HCWs from general wards were collected and processed by standard laboratory procedures.
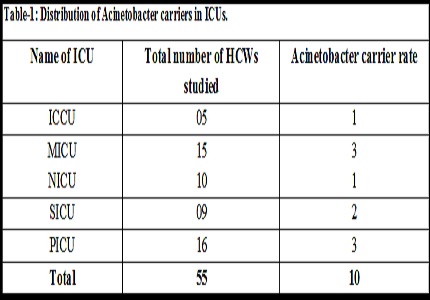
Results: Prevalence of A. baumanii carriers was 18.18%. Higher carrier rate was observed in male than female HCWs (12.72% Vs 5.5%). carrier rate was 22.2% and 18.75% in SICU and PICU respectively with none from general wards. Carrier rate was 7.3% at axilla and hands.
Conclusion: Colonization of hospitalized patients play an important role in subsequent colonization of hands of hospital staff during trivial contacts, there by contributing to the spread and persistence of outbreaks.
Downloads
References
2. Rungrunghiranya S, Somboonwit C, Kanchanapoom T. Acinetobacter infection in the intensive care unit. J Infect Dis Antimicrob Agents 2005; 22(2):77-92.
3. Fallon RJ, Young H, Neisseria, Moraxella, Acinetobacter. In: Collee JG, editor. Mackie and McCartney Practical Medical Microbioligy. 14th ed. Edinburg: Churchill Livingstone; 2006.p.294-6.
4. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Seventeenth Informational Supplement. CLSI document M 100-S 17. Vol. 27. Suppl. 17. Wayne, Pa: Clinical and Laboratory Standards; 2007.
5. Lee BY, McGlone SM, Doi y, Bailey RR, Harrison LH. Economic value of Acinetobacter baumanii screening in the intensive care unit. Clinical Microbiology and Infection: the official publication of the Europian Society of Clinical Microbiology and infectious Diseases 2011;17(11):1691-1697.
6. Bergogne-Bérézin E, Towner KJ. Acinetobacter spp. as nosocomial pathogens: microbiological, clinical, and epidemiological features. Clin Microbiol Rev. 1996 Apr;9(2):148-65.
7. Marchaim D, Navon-venezia S, Schwartz D, Tarabeia J, Fefer I, Schwaber M, et al. Surveillance cultures and duration of carriage of multidrug- resistant Acinetobacter baumanii. American Society for Microbiology Journal of Clinical Microbiology 2007;45(5):1551-1555.
8. Joseph NM, Sistla S, Dutta TK, Badhe AS, Rasitha D, Parija SC. Role of intensive care unit environment and health-care workers in transmission of ventilator-associated pneumonia. J Infect Dev Ctries. 2010 Jun 3;4 (5): 282-91. [PubMed]
9. Morgan DJ, Liang SY, Smith CL, et al. Frequent Multidrug-Resistant Acinetobacter baumanii Contamination of Gloves, and Hands of Healthcare Workers. Infect Control Hosp Epidemiol: the official journal of the Soceity of Hospital Epidemiologists of America.2010;31(7):716-721. Doi:10.1086/653201.
10. Bayuga S, Zeana C, Sahni J, Delta-Latta P, el-sadrw, Larson E. Prevalence and antimicrobial pattern of Acinetobacter baumanii on hands and nares of hospital personnel and patients: The iceberg phenomenon again. Heart Lung 2002;31:382-90.
11. R. Morfín-Otero, M. D. Alcántar-Curiel, M. J. Rocha, C. M. Alpuche-Aranda, J. I. Santos-Preciado, C. Gayosso-Vázquez, J. R. Araiza-Navarro, M. Flores-Vaca, S. Esparza-Ahumada, E. González Díaz, et al. Acinetobacter baumanii infections in a tertiary care hospital in Mexico over the past 13 years. Chemotherapy 2013;59:57-65.doi: 10.1159/000351098. [PubMed]


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


