Microbiological profile and antimicrobial susceptibility pattern of chronic suppurative otitis media in a tertiary care centre
Abstract
Introduction: Chronic suppurative otitis media (CSOM) is a common clinical condition diagnosed in ENT out patients department (OPD). There appears paucity of data on the incidence and pattern of bacterial and fungal flora in patients presenting with ear discharge.
Materials and Methods: A total of 180 consecutive patients with CSOM attending the ENT OPD of a tertiary care hospital in North India were included in the study. 3 swabs were used to collect the ear discharge and were processed for isolation of bacterial and fungal organisms. The bacterial isolates thus obtained were tested for antibiotic susceptibility testing. Isolates of Staphylococcus aureus were also tested for methicillin resistance. Fungal growth was identified and antifungal sux sceptibility testing of yeast isolates was done using standard recommended procedures.
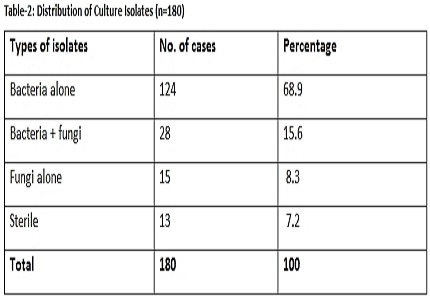
Results: Microbiological profile of total 180 cases revealed, bacteria alone in 68.9% cases, bacteria along with fungi in 15.6% cases and fungi alone in 8.3% cases. Amongst these, Pseudomonas aeruginosa was the most common bacterium isolated (34.9%) followed by Staphylococcus aureus (24.4%). Out of the fungal isolates obtained, Aspergillus nigerwas the commonest isolate (29.4%) followed by Candida albicans(19.5%). MRSA strains were 37%. Among the Pseudomonas aeruginosa isolates, maximum resistance was found to Ciprofloxacin (74.2%) followed by Gentamicinand Ceftazidime. All Candida species were sensitive to Fluconazole, Itraconazole and Voriconazole.
Conclusion: Considering the emergence of bacterial resistance and the availability of wide spectrum of newer antimicrobial agents, it is important to know the pattern of infections and the antimicrobial sensitivity of the isolates.
Downloads
References
2. Iseh KR, Adegbite T. Pattern and bacteriology of acute suppurative otitis media in Sokoto, Nigeria. Annals of African Medicine 2004;3(4):164-66. [PubMed]
3. Couzos S, Lea T, Mueller R, Murray R, Culbong M. Effectiveness of ototopicalantibiotics for chronic suppurative otitis media in Aboriginalchildren: a community-based, multicentre, double-blindrandomised controlled trial. Med J Aust. 2003 Aug 18;179(4):185-90. [PubMed]
4. El-sayed Y. Bone conduction impairment in uncomplicated CSOM. Am J Otolaryngol.1998;19:149-53.
5. Rao BN and Reddy MS. Chronic Suppurative Otitis Media – A prospective Study. Indian Journal of Otolaryngology and Head Neck Surgery 1994;3:72-7. [PubMed]
6. Bluestone CD. Otitis media; to treat or not to treat. Consultant 1998:1421–33.
7. Block SL. Causative Pathogens, antibiotic resistance and Therapeutic Considerations in Otitis media. Paediatr Infect Dis J 1997;16:449-456.
8. Mittal A. Secondary fungal infections in chronic suppurative otitis media. IJO & HNS 1997:49(2):112-6.
9. Aich ML, Biswas AC, Ahmed M, Joarder MAH, Datta PG, Alauddin M. Prevalence of Otitis media with effusion among school going children in Bangladesh. Bangladesh J Otorhinolaryngol2009;15:31-34. [PubMed]
10. Nowak K, Szyfter W. [Problematics of fungal infections in the ear]. Otolaryngol Pol. 2008;62(3):254-60. doi: 10.1016/S0030-6657(08)70250-6.
11. Performance Standards for antimicrobial susceptibility testing; Clinical and laboratory standards institute. Eighteenth Informational supplement. 2008;28(1): M100-S18.
12. Milne LJR. Fungi. In: Mackie and McCartney Practical Microbiology. 14th ed. New York: churchill Livingstone; 1999.p.695-717.
13. Forbes BA, Sahm DF and Weissfeld AS. Laboratory Methods in Basic Mycology. In: Bailey and Scott's Diagnostic Microbiology. 11th ed. St. Louis: Mosby; 2002.p.711-798.
14. Winn WC, Koneman EW, Allen SD, IIle Y. Mycology. In:Koneman'sColour Atlas and Textbook of Diagnostic Microbiology. 6th ed. Philadelphia: Lipincott Williams & Williams; 2006.p.1153-232.
15. National Committee for Clinical Laboratory Standards. Methods for Antifungal Disc Diffusion Susceptibility Testing of Yeast: Approved Guideline M44-A.Wayn, PA: National committee for clinical laboratory standars: 2004. [PubMed]
16. Ingroff AE, Canton E, Gibbs D, Wang A. correlation of Neo-sensitabs tablet diffusion assey results on three different agar media with CLSI broth microdilution M27-A2 and disk diffusion M44-A results for testing susceptibilities of Candida species and Cryptococcus neoformans to Amphotericin-B, Caspofungin, Fluconazole, Itraconazole and Voriconazole. Journal of clinical microbiology 2007;858-64. [PubMed]
17. Pfaller MA, Boyken I, Messer SA, Tendikor s, Hollis Rj et al. Comparision results of Voriconazole disk diffusion testing from a central reference laboratory in the AREMIS global antifungal surveillance program. Journal of clinical microbiology 2005;5208-13. [PubMed]
18. Jackler RK, Kaplan MJ. Ear, Nose and Throat. In: Current Medical Diagnosis and Treatment 46th ed. New York: Mc Graw-Hill:2007. p.184-9
19. Kumar H, Seth S. Bacterial and fungal study of 100 cases of chronic suppurative otitis media.JClinDiagn Res 2011;5: 1224-7. [PubMed]
20. Indudharan R, Haq JA, Aiyar S. Antibiotics in chronic suppurative otitis media: a bacteriologic study. Ann OtolRhinolLaryngol. 1999 May;108(5):440-5.
21. Maji PK. The investigation of bacteriology of chronic suppurative otitis media in patients attending a tertiary care hospital with special emphasis on seasonal variation. Indian J. otolaryngol. Head neck surg.2007;59:128-31.
22. Agrawal A, Kumar D, Goyal A, Singh N, Khandelwal G. Microbiological profile and their antimicrobial sensitivity pattern in patients of otitis media with ear discharge. Indian J Otol 2013; 19:5-8.
23. Baruah PC, Agarwal SC, Arora MML, Mehra YN. Ind J Otolaryngology;1972(24):157. [PubMed]
24. Hiremath SL, Kantar C,YeshwanthraoM,Vasantha Kumar CM. Aerobic Bacterial Isolates of CSOM and Their Antibiotic Sensitivity Pattern. The Indian Practitioner.2001;54(7):484-9. [PubMed]
25. Bairy I, Pradhan D, Yenigalla BM. Microbiology of Chronic Suppurative Otitis Media. Indian Journal of Otology;2007(13):21-4.
26. Gulati J, Tendon PL, Singh W and Bais AS. Study of Bacterial Flora in Chronic Suppurative Otitis Media. Ind. J. Otolaryngology;1969(21):198.
27. Olusesi AD. Otitis media as a cause of significanthearing loss among Nigerians.Int JPediatrOtorhinolaryngol. 2008 Jun;72(6):787-92. doi: 10.1016/j.ijporl.2008.02.008. Epub 2008 Apr 2.
28. Rupa V, Jacob A, Joseph A. Chronicsuppurative otitis media: prevalence and practices among ruralSouthIndianchildren. Int JPediatrOtorhinolaryngol. 1999 May 25;48(3):217-21. [PubMed]
29. Mohan U, Jindal N. Fungal and bacterial flora of chronic suppurative otitis media in Amritsar (Punjab). IJO & HNS. 1998;50(2):175-7.
30. Akinpelu OV, Amusa YB, Komolafe EO, Adeolu AA, Oladele AO, Ameye SA. Challenges in management of chronicsuppurative otitis media in a developing country. J Laryngol Otol. 2008 Jan;122(1):16-20. Epub 2007 May 22. [PubMed]
31. WHO/CIBA Foundation Workshop. Prevention of hearing impairment from chronic otitis media. WHO/PDH/98.4 London: CIBA Foundation, 1996.
32. Mann SBS, Grewal BS, Nahar MS. Incidence of Chronic Suppurative Otitis Media in general population. Ind Jour Otolaryng1976;28:35-40. [PubMed]
33. Ballal M. Chronic suppurative otitis media- a bacteriological and mycological study. Ind J of Otolaryngology and Head and Neck Surgery 1992;1(1):10-3.
34. Sree Rama Rao K, Manjaneyulu P. Otomycosis. Ind Journal of Otolaryngology 1979;31:65-8.
35. Sen Gupta RP, Kacker SK. OtomycosisIndian J Med Sci. 1978 Jan-Feb;32(1-2):5-7. [PubMed]
36. Mawson SR, Ludman H. Diseases of the ear. London: Edward Arnold; 1979.p.267-8, 334-47.
37. Ravichandra Prakash H, BeloduR,Karangate N, Sonth S, Anitha.M.R, Vijayanath. V. Antimicrobial susceptibility pattern of Pseudomonas aeruginosa strains isolated from clinical sources. Journal of Pharmaceutical and Biomedical Sciences 2012; 14 (5):1-4. [PubMed]
38. Rex JH, Pfaller MA, Walsh TJ, Chaturvedi V, Espinel-Ingroff A, Ghannoum MA, Gosey LL, Odds FC, Rinaldi MG, Sheehan DJ, Warnock DW. Antifungalsusceptibilitytesting: practicalaspects and currentchallenges. ClinMicrobiol Rev. 2001 Oct;14(4):643-58, table of contents.
39. Pfaller MA, Diekema BJ, Gibbs DL et al. Results from the Artemis Disc Global Antifungal Surveillance Study, 1997-2005: An 8.5 year Analysis of Susceptibilities of C. species and other Yeast Species to Fluconazole and Voriconazole determined by CLSI Standarized Disc Diffusion Testing. Journal of Clinical Microbiology 2007;45:1735-45.
40. Matar MJ, Zeichner LO, Paetznick VL, Rodriguez JR, Chen E, Rex JH. Correlation between E-Test Disc Diffusion and Microdilution Methods for Antifungal Susceptibility testing of fluconazole and voriconazole. Antimicrobial agents and chemotherapy.2003;47(5):1647-51. [PubMed]
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


