Histopathological study of ovarian lesions at a tertiary rural hospital
Gaikwad SL.1, Badlani KS.2*, Birare SD.3
DOI: https://doi.org/10.17511/jopm.2020.i03.06
1 Sheela Lakshmanrao Gaikwad, Associate Professor, Swami Ramanand Teerth Rural Government Medical College, Ambajogai, Maharashtra, India.
2* Koshu Sitaram Badlani, Post-graduate, Swami Ramanand Teerth Rural Government Medical College, Ambajogai, Maharashtra, India.
3 Shivaji Dadarao Birare, Professor, Swami Ramanand Teerth Rural Government Medical College, Ambajogai, Maharashtra, India.
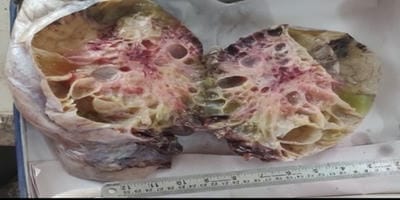
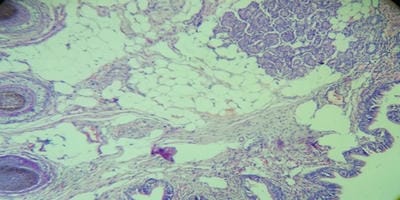
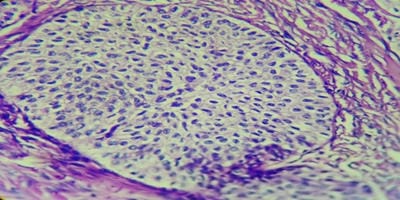
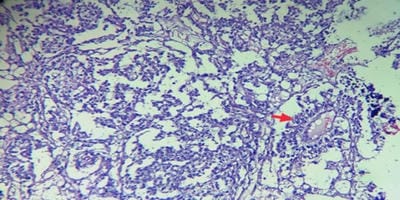
Background:Ovaries are the third leading site of cancer among women trailing behind cervical and breast cancer according to the Indian cancer registries. The spectrum of ovarian lesions is wide with harmless simple cystic lesions at one end and the fatal aggressive malignant lesions at the other end. Thus, ovarian neoplasm offers a good field for research. Methods: This was a prospective two years observational study and was conducted at the Department of Pathology SRTR GMC, Ambajogai, including 185 ovarian lesions. Result: Total 185 ovarian lesions were studied, 101 cases were non-neoplastic while 84 cases were neoplastic. The most common non-neoplastic lesion was corpus luteal cyst (27.7%) followed by simple ovarian cyst (24.7%) and follicular cyst (21.8%). Among 84 neoplastic cases, 74 cases (88.1%) were benign,02 cases (2.4%) were borderline tumours and 08 cases (9.5%) were diagnosed malignant. Conclusions: Both non-neoplastic as well as neoplastic lesions of ovary often present with similar clinical and radiological features. So histopathological study is essential to diagnose ovarian tumours and predict their prognosis.
Keywords: Ovarian Lesions, Non-Neoplastic, Neoplastic, Histopathological Study
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Post-graduate, Swami Ramanand Teerth Rural Government Medical College, Ambajogai, Maharashtra, India. Email: |
Gaikwad SL, Badlani KS, Birare SD. Histopathological study of ovarian lesions at a tertiary rural hospital. Trop J Pathol Microbiol. 2020;6(3):245-252. Available From https://pathology.medresearch.in/index.php/jopm/article/view/441 |


 ©
©