A Rare Case of Rhinosporidiosis in Popliteal Fossa
Gupta R.1, Saishruti.2*
DOI: https://doi.org/10.17511/jopm.2021.i03.04
1 Ranu Gupta, M.D., Department of Pathology, Consultant Pathologist, Centrapath laboratory, Indore, Madhya Pradesh, India.
2* Saishruti, M.D., Department Microbiology, Dr Lalpathlabs, Hyderabad, Telangana, India.
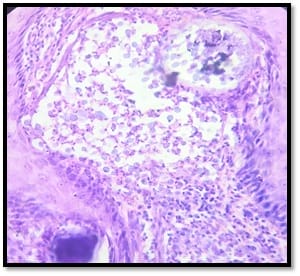
We hereby present a rare case of rhinosporidiosis in the popliteal fossa. Rhinosporidiosis is a chronic granulomatous infection caused by the fungus-like organism Rhinosporidium seebrii most commonly in the nasal cavity, followed by ocular and cutaneous lesions. The following case is of a 45-year-old female who presented to the laboratory with a pedunculated mass which on histopathology revealed a typical sporangium with numerous endospores. The report provides an insight into the clinical suspicion that needs to be kept while handling such cases.
Keywords: Rhinosporidium seebrii, Pedunculated mass, Popliteal fossa
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , M.D., Department Microbiology, Dr Lalpathlabs, Hyderabad, Telangana, India. Email: |
Gupta R, Saishruti. A Rare Case of Rhinosporidiosis in Popliteal Fossa. Trop J Pathol Microbiol. 2021;7(3):116-118. Available From https://pathology.medresearch.in/index.php/jopm/article/view/516 |


 ©
©