Inducible Clindamycin Resistance in Staphylococcus aureus isolated from pus samples in an Orthopaedic tertiary care centre.
Pratibha S.1*, Kumar P.2
DOI: https://doi.org/10.17511/jopm.2021.i01.08
1* Pratibha S, Assistant Professor, Department of Microbiology, Sanjay Gandhi Institute of Trauma and Orthopedics, Bangalore, Karnataka, India.
2 Praveen Kumar, Senior Technician, Department of Microbiology, Sanjay Gandhi Institute of Trauma and Orthopedics, Bangalore, Karnataka, India.
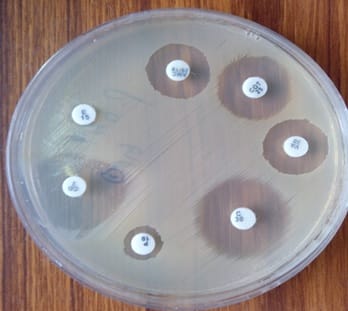
Introduction: Clindamycin is a commonly used antibiotic to treat skin and soft tissue infections caused by Staphylococcus aureus particularly Methicillin-Resistant Staphylococcus aureus (MRSA) infection. In vitro routine tests for clindamycin susceptibility may fail to detect inducible clindamycin resistance due to genes resulting in treatment failure, thus necessitating the need to detect such resistance by a simple D - test on a routine basis. Materials and Methods: 165 isolates of Staphylococcus aureus were subjected to routine antibiotic susceptibility testing including Oxacillin (1µg) and Cefoxitin (30µg) by Kirby Bauer disc diffusion method. Inducible clindamycin resistance was detected by D test as per CLSI guidelines on erythromycin resistant isolates. Results: 24 (14.5%) isolates showed inducible clindamycin resistance, 8 (4.84%) showed constitutive resistance while the remaining 59 (35.75%) showed MS phenotype. Inducible clindamycin resistance and MS phenotype were found higher in MRSA (21.42%, 40.47%) as compared to MSSA (7.40%, 30.86%). Conclusion: This study showed that the D test should be used as a mandatory method in routine disc diffusion testing to detect inducible clindamycin resistance.
Keywords: Inducible, Constitutive, MS phenotype, MRSA, MSSA
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Microbiology, Sanjay Gandhi Institute of Trauma and Orthopedics, Bangalore, Karnataka, India. Email: |
Pratibha S, Kumar P. Inducible Clindamycin Resistance in Staphylococcus aureus isolated from pus samples in an Orthopaedic tertiary care centre.. Trop J Pathol Microbiol. 2021;7(1):50-54. Available From https://pathology.medresearch.in/index.php/jopm/article/view/509 |


 ©
©