A retrospective study on histomorphological spectrum of ovarian lesions in a tertiary care hospital
Subashree K.1*, Ravindran S.2, Balaji S.3
DOI: https://doi.org/10.17511/jopm.2020.i07.03
1* Subashree K., Assistant Professor, Department of Pathology, Sri Venkateshwaraa Medical College and Research Centre, Puducherry, India.
2 Sneha Ravindran, Post-graduate, Department of Pathology, Sri Venkateshwaraa Medical College and Research Centre, Puducherry, India.
3 Balaji S., Post-graduate, Department of Pathology, Sri Venkateshwaraa Medical College and Research Centre, Puducherry, India.
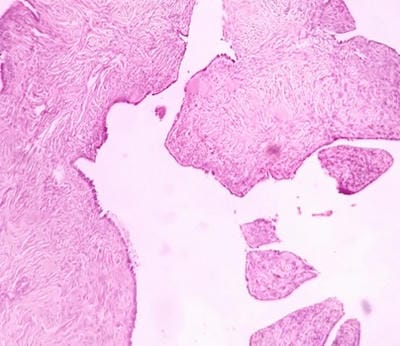
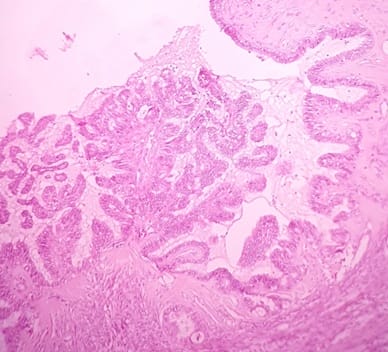
Introduction: Gynecological morbidity is defined as any condition, disease, or dysfunction of the reproductive system which is not related to pregnancy, abortion, or childbirth. A significant number of ovarian lesions have been known to cause Gynecological morbidity among most females. With the increased use of screening modalities, ovarian lesions have increasingly been encountered for pathological analysis. It is important to evaluate the pattern of clinical presentation, corroborating with histological diagnosis. Purpose: The present study was carried out to evaluate the histomorphological spectrum of various ovarian lesions among women in Puducherry. Material and Methods: This retrospective study was conducted on 350 ovarian samples received for five years in the Department of Pathology, of our tertiary teaching hospital. Clinicopathological data were retrieved from the hospital records. The histomorphological analysis was reviewed and neoplastic and non-neoplastic ovarian lesions were segregated according to the World Health Organization classification. Results: Based on histology, the predominant ovarian lesions diagnosed were non-neoplastic conditions including simple and follicular cyst, corpus luteal cyst, corpus hemorrhagic cyst, and cystic follicles constituting 40.6% on the right side and 34% on the left side. Malignancy was predominant on the right side (1.7%) while the same was 0.6% on the left side. Conclusion: The present study has identified that non-neoplastic lesions are more common in ovaries than neoplastic lesions and it has identified that serous cystadenomas are the most common ovarian neoplastic lesions.
Keywords: Histomorphological patterns, Ovarian lesion, Neoplastic lesions, Non-neoplastic lesions, Ovary
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Pathology, Sri Venkateshwaraa Medical College and Research Centre, Puducherry, India. Email: |
Subashree K, Ravindran S, Balaji S. A retrospective study on histomorphological spectrum of ovarian lesions in a tertiary care hospital. Trop J Pathol Microbiol. 2020;6(7):430-436. Available From https://pathology.medresearch.in/index.php/jopm/article/view/488 |


 ©
©