Histopathological spectrum of Cervical Lesion”– two and half Year prospective Study in Tertiary Care Center of Chhattisgarh, India
Kujur P.1, Indoria C.2*, Bagde S.3, Tiwari A.4
DOI: https://doi.org/10.17511/jopm.2021.i02.01
1 Pratima Kujur, Professor, Department of Pathology, BRLSABVM Government Medical College, Rajnandgaon, Chhattisgarh, India.
2* Chandrashekhar Indoria, Assistant Professor, Department of Pathology, BRLSABVM Government Medical College, Rajnandgaon, Chhattisgarh, India.
3 S. Bagde, Associate Professor, Department of Pathology, BRLSABVM Government Medical College, Rajnandgaon, Chhattisgarh, India.
4 A. Tiwari, Assistant Professor, Department of Pathology, BRLSABVM Government Medical College, Rajnandgaon, Chhattisgarh, India.
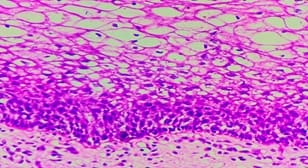
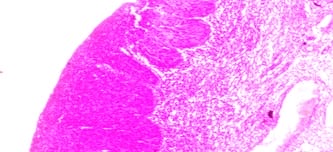
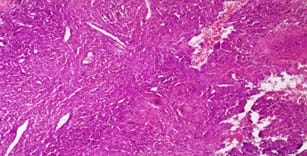
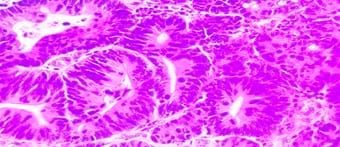
Introduction: Cervical lesions are the leading cause of morbidity in Indian women and cervical cancer is the second most common cancer in women worldwide next to breast cancer. Objectives: To study the age distribution, the relative frequency of various cervical lesions and histopathological features of cervical lesions. Materials and Methods: This is a two & half years retrospective study of all cervical biopsies and hysterectomy specimens received from September 2017 to March 2020 in the department of pathology. Result: In a total of 485 cases studied 359 (74.1%) cases were non-neoplastic, 107(22%) were preinvasive and 19 (3.9%) cases were malignant. Cervicitis was the most common non-neoplastic lesion and squamous cell carcinoma was the most common cancer. Conclusion: Our study highlights a vast spectrum of cervical lesions and therefore early detection and management of certain lesions can help in reducing morbidity.
Keywords: Cervical lesions, Histology and pathology, Carcinoma cervix
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Pathology, BRLSABVM Government Medical College, Rajnandgaon, Chhattisgarh, India. Email: |
Kujur P, Indoria C, Bagde S, Tiwari A. Histopathological spectrum of Cervical Lesion”– two and half Year prospective Study in Tertiary Care Center of Chhattisgarh, India. Trop J Pathol Microbiol. 2021;7(2):65-70. Available From https://pathology.medresearch.in/index.php/jopm/article/view/487 |


 ©
©