Epidemiological and histopathological study of thyroid lesions in a tertiary care hospital in south India
Chandana A.1, Gomathi R.2*, Prakashiny S.3
DOI: https://doi.org/10.17511/jopm.2020.i06.03
1 Adayalam Chandana, Assistant Professor, Department of Pathology, Sri Balaji Vidyapeeth Deemed to be University, Kancheepuram, Tamil Nadu, India.
2* Gomathi R., Associate Professor, Department of Pathology, Sri Balaji Vidyapeeth Deemed to be University, Kancheepuram, Tamil Nadu, India.
3 Prakashiny S., Assistant Professor, Department of Pathology, Sri Balaji Vidyapeeth Deemed to be University, Kancheepuram, Tamil Nadu, India.
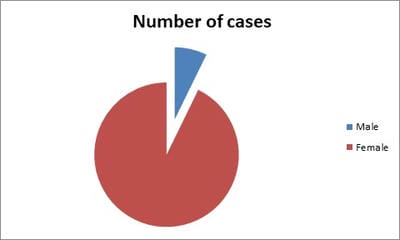
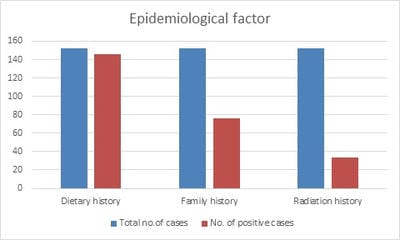
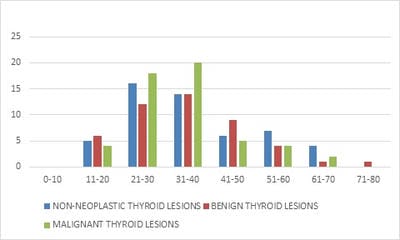
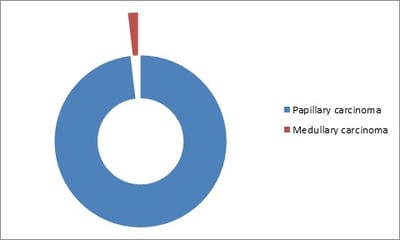
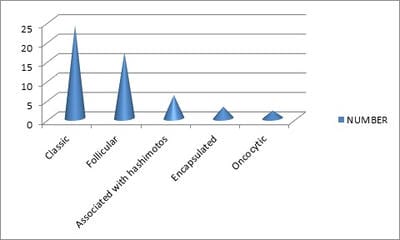
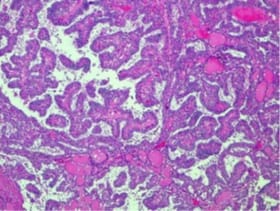
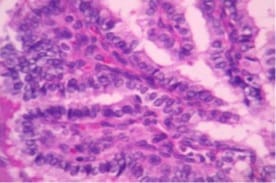
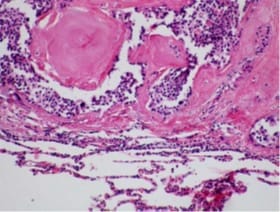
Introduction: Thyroid swellings are easily picked up on general physical examination. Due to various cosmetic concerns, there has been a steady increase in thyroid surgeries in recent years. Many epidemiological risk factors have been attributed to the development of various thyroid lesions and malignancies. The present study was carried out to evaluate the epidemiology and histopathological distribution of various thyroid lesions. Material and Methods: This cross-sectional study was carried out among 130 patients presenting with visible thyroid swelling to our tertiary care institution. The post-operative specimens of the thyroid were fixed in 10% formalin, processed, embedded in paraffin blocks, 3-5μm sections cut and stained with Hematoxylin and Eosin. Results: Out of the 152 cases of thyroid lesions analyzed, 12 (7.9%) were simple goiter, 15(9.9%) were multinodular goiter, 47 (30.9%) were adenomas, 52 (34.2%) were papillary carcinomas, 1 (0.6%) was medullary carcinoma. About 96% of the participants had a positive dietary history, 50% of them had a positive family history. Papillary carcinoma and its variants were the most commonly diagnosed lesion accounting for about 34.2% of the cases. Conclusion: Thyroid biopsy rates are on the rise because of increased awareness. Therefore, the detection of thyroid malignancies is also on the rise. The diagnosis and management of thyroid tumors require a collective outlook on the part of the clinician and pathologist. Despite advances in imaging technology pathologists’ role is very important in the diagnosis of thyroid neoplasms and in predicting the prognosis and patient outcome.
Keywords: Thyroid malignancy; Microscopic variants, Papillary carcinoma, Thyroid nodules
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Pathology, Sri Balaji Vidyapeeth Deemed to be University, Kancheepuram, Tamil Nadu, India. Email: |
Chandana A, Gomathi R, Prakashiny S. Epidemiological and histopathological study of thyroid lesions in a tertiary care hospital in south India. Trop J Pathol Microbiol. 2020;6(6):381-386. Available From https://pathology.medresearch.in/index.php/jopm/article/view/468 |


 ©
©