Paraganglioma of the urinary bladder
Fatima S.1*, Mahdy O.2, Wajih S.S.3
DOI: https://doi.org/10.17511/jopm.2020.i04.11
1* Sohaila Fatima, Assistant Professor, Department of Pathology, King Khalid University, Abha, Saudi Arabia.
2 Omaia Mahdy, Specialist, Department of Laboratory Medicine, Aseer Central Hospital, Abha, Saudi Arabia.
3 Shiza Wajih Siddiqui, Medical Student, Dubai Medical College, United Arab Emirates.
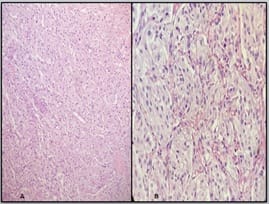
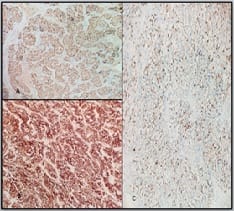
Paragangliomas are extra-adrenal pheochromocytomas. They are catecholamine-secreting neoplasms developing from the chromaffin cells derived from the ectodermic neural system. They are rare neoplasms that account for less than 0.06% of all urinary bladder tumors and 6% of all extra-adrenal pheochromocytomas. They arise from chromaffin tissue of the sympathetic nervous system within the layers of the bladder wall. They can be present in any part of the bladder with a predilection for the detrusor muscle with the most common sites being the dome and trigone.They may be nonfunctional or functional. The most common symptoms are hypertension and hematuria. Functional tumors usually present with symptoms of excessive catecholamine secretion. The patient typically suffers from hypertensive crises that may be accompanied by headache, palpitations, hot flushes, and sweating. Postmicturition hypotension and syncope are another common presentations. They share a genetic basis and can be related to a number of hereditary conditions.They are usually benign but there are no reliable morphologic criteria by which to separate the benign from the malignant forms. Here we present a 22 years old female with hematuria which on histopathology proved to be paraganglioma of the urinary bladder.
Keywords: Paragangliomas, Extra-adrenal pheochromocytomas, Urinary bladder
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Pathology, King Khalid University, Abha, Saudi Arabia. Email: |
Fatima S, Mahdy O, Siddiqui SW. Paraganglioma of the urinary bladder. Trop J Pathol Microbiol. 2020;6(4):333-335. Available From https://pathology.medresearch.in/index.php/jopm/article/view/449 |


 ©
©